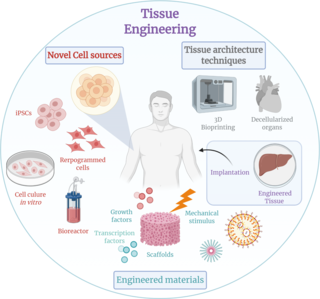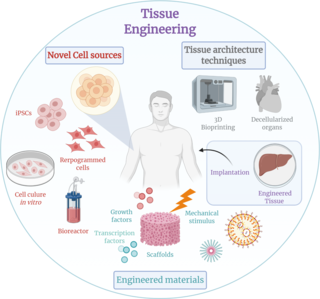
Tissue engineering is a biomedical engineering discipline that uses a combination of cells, engineering, materials methods, and suitable biochemical and physicochemical factors to restore, maintain, improve, or replace different types of biological tissues. Tissue engineering often involves the use of cells placed on tissue scaffolds in the formation of new viable tissue for a medical purpose, but is not limited to applications involving cells and tissue scaffolds. While it was once categorized as a sub-field of biomaterials, having grown in scope and importance, it can is considered as a field of its own.

Bioglass 45S5 or calcium sodium phosphosilicate, is a bioactive glass specifically composed of 45 wt% SiO2, 24.5 wt% CaO, 24.5 wt% Na2O, and 6.0 wt% P2O5. Typical applications of Bioglass 45S5 include: bone grafting biomaterials, repair of periodontal defects, cranial and maxillofacial repair, wound care, blood loss control, stimulation of vascular regeneration, and nerve repair.

A biomaterial is a substance that has been engineered to interact with biological systems for a medical purpose – either a therapeutic or a diagnostic one. The corresponding field of study, called biomaterials science or biomaterials engineering, is about fifty years old. It has experienced steady growth over its history, with many companies investing large amounts of money into the development of new products. Biomaterials science encompasses elements of medicine, biology, chemistry, tissue engineering and materials science.
Nano-scaffolding or nanoscaffolding is a medical process used to regrow tissue and bone, including limbs and organs. The nano-scaffold is a three-dimensional structure composed of polymer fibers very small that are scaled from a Nanometer scale. Developed by the American military, the medical technology uses a microscopic apparatus made of fine polymer fibers called a scaffold. Damaged cells grip to the scaffold and begin to rebuild missing bone and tissue through tiny holes in the scaffold. As tissue grows, the scaffold is absorbed into the body and disappears completely.
A fibrin scaffold is a network of protein that holds together and supports a variety of living tissues. It is produced naturally by the body after injury, but also can be engineered as a tissue substitute to speed healing. The scaffold consists of naturally occurring biomaterials composed of a cross-linked fibrin network and has a broad use in biomedical applications.
Nick Rhodes is a Reader in Tissue Engineering and Regenerative Medicine at the University of Liverpool, in the U.K. Tissue Engineering can be described as the use of engineering techniques, including engineering materials and processes, in order to grow living tissues. Regenerative Medicine can be described as the treatment of defective tissues using the regenerative capacity of the body's healthy tissues. Rhodes describes the discipline as "aiming to repair tissue defects by driving regeneration of healthy tissues using engineered materials and processes."
Kristi S. Anseth is the Tisone Distinguished Professor of Chemical and Biological Engineering, an Associate Professor of Surgery, and a Howard Hughes Medical Investigator at the University of Colorado at Boulder. Her main research interests are the design of synthetic biomaterials using hydrogels, tissue engineering, and regenerative medicine.

Gordana Vunjak-NovakovicFRSC is a Serbian American biomedical engineer and university professor. She is a University Professor at Columbia University, as well as the Mikati Foundation Professor of Biomedical Engineering and Medical Sciences. She also heads the laboratory for Stem Cells and Tissue Engineering at Columbia University. She is part of the faculty at the Irving Comprehensive Cancer Center and the Center for Human Development, both found at Columbia University. She is also an honorary professor at the Faculty of Technology and Metallurgy at the University of Belgrade, an honorary professor at the University of Novi Sad, and an adjunct professor at the Department of Biomedical Engineering at Tufts University.

Decellularization is the process used in biomedical engineering to isolate the extracellular matrix (ECM) of a tissue from its inhabiting cells, leaving an ECM scaffold of the original tissue, which can be used in artificial organ and tissue regeneration. Organ and tissue transplantation treat a variety of medical problems, ranging from end organ failure to cosmetic surgery. One of the greatest limitations to organ transplantation derives from organ rejection caused by antibodies of the transplant recipient reacting to donor antigens on cell surfaces within the donor organ. Because of unfavorable immune responses, transplant patients suffer a lifetime taking immunosuppressing medication. Stephen F. Badylak pioneered the process of decellularization at the McGowan Institute for Regenerative Medicine at the University of Pittsburgh. This process creates a natural biomaterial to act as a scaffold for cell growth, differentiation and tissue development. By recellularizing an ECM scaffold with a patient’s own cells, the adverse immune response is eliminated. Nowadays, commercially available ECM scaffolds are available for a wide variety of tissue engineering. Using peracetic acid to decellularize ECM scaffolds have been found to be false and only disinfects the tissue.
The in vivo bioreactor is a tissue engineering paradigm that uses bioreactor methodology to grow neotissue in vivo that augments or replaces malfunctioning native tissue. Tissue engineering principles are used to construct a confined, artificial bioreactor space in vivo that hosts a tissue scaffold and key biomolecules necessary for neotissue growth. Said space often requires inoculation with pluripotent or specific stem cells to encourage initial growth, and access to a blood source. A blood source allows for recruitment of stem cells from the body alongside nutrient delivery for continual growth. This delivery of cells and nutrients to the bioreactor eventually results in the formation of a neotissue product.
Brian Derby FIMMM is professor of materials science at Manchester University. He has been at the forefront of research into inkjet printing and 3D bioprinting, winning the Edward de Bono Medal for Original Thinking in 2007 for his work on Printing Skin and Bones: using inkjet printing technology to fabricate complex tissue scaffolds on which cells can be grown.
Treena Livingston Arinzeh is an American biomedical engineer and academic.

Aline Fiona Miller is a Professor of Biomolecular Engineering at the University of Manchester. She specialises in the characterisation of polymer, biopolymer and peptides, using neutron and x-ray scattering, as well as the development of functionalised nanostructures for regenerative medicine and toxicology testing.
Sarah Harriet Cartmell is a British biomaterials scientist and Professor of Bioengineering at the University of Manchester. She specializes on the potential use of electrical regimes to influence cellular activity for orthopaedic tissue engineering applications.
Susmita Bose is an Indian-American scientist and engineer, best known for her research on biomaterials, 3D printing or additive manufacturing of bone implants and natural medicine. She is the Herman and Brita Lindholm Endowed Chair Professor in the School of Mechanical and Materials Engineering at Washington State University.

Milica Radisic is a Serbian Canadian tissue engineer, academic and researcher. She is a professor at the University of Toronto’s Institute of Biomaterials and Biomedical Engineering, and the Department of Chemical Engineering and Applied Chemistry. She co-founded TARA Biosystems and is a senior scientist at the Toronto General Hospital Research Institute.
Elizabeth Cosgriff-Hernandez is an American biomedical engineer who is a professor at the University of Texas at Austin. Her work involves the development of polymeric biomaterials for medical devices and tissue regeneration. She is a co-founder of Rhythio Medical, on the scientific advisory board of ECM Biosurgery, and a consultant to several companies on biostability evaluation of medical devices. Dr. Cosgriff-Hernandez is an associate editor of the Journal of Materials Chemistry B and Fellow of the International Union of Societies for Biomaterials Science and Engineering, Biomedical Engineering Society, Tissue Engineering and Regenerative Medicine International Society, American Chemical Society Division of Polymeric Materials: Science and Engineering, Royal Society of Chemistry, and the American Institute for Medical and Biological Engineering.
Helen Haiyan Lu is a Chinese American biomedical engineer and the Percy K. and Vida L. W. Hudson professor of biomedical engineering at the Columbia University Fu Foundation School of Engineering and Applied Science. Her work focuses on understanding and developing therapies in complex tissue systems, especially the interface between soft tissue and bone.
Tatiana Segura is an American biomedical engineer who is a professor at Duke University. Her research considers biomedical engineering solutions to promote cell growth. She was elected Fellow of the American Institute for Medical and Biological Engineering in 2017 and awarded the Acta Biomaterialia Silver Medal in 2021.
Hala Zreiqat is a biomechanical engineer whose research focuses on the development of novel engineered synthetic materials and 3D printed platforms for regenerative medicine. She is a Payne-Scott Professor in the Department of Biomechanical Engineering at the University of Sydney.