Dilationand curettage (D&C) refers to the dilation (widening/opening) of the cervix and surgical removal of part of the lining of the uterus and/or contents of the uterus by scraping and scooping (curettage). It is a gynecologic procedure used for diagnostic and therapeutic purposes, and is the most commonly used method for first-trimester miscarriage or abortion.

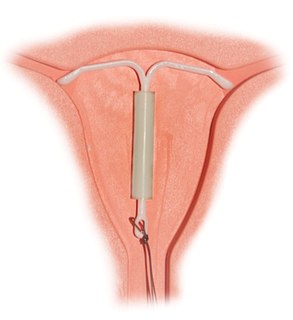
Intrauterine device (IUD) with copper, also known as intrauterine coil, is a type of intrauterine device which contains copper. It is used for birth control and emergency contraception within five days of unprotected sex. It is one of the most effective forms of birth control with a one-year failure rate around 0.7%. The device is placed in the uterus and lasts up to twelve years. It may be used by women of all ages regardless of whether or not they have had children. Following removal, fertility quickly returns.

Emergency contraception (EC) is a birth control measure, used after sexual intercourse to prevent pregnancy.

Ectopic pregnancy is a complication of pregnancy in which the embryo attaches outside the uterus. Signs and symptoms classically include abdominal pain and vaginal bleeding, but fewer than 50 percent of affected women have both of these symptoms. The pain may be described as sharp, dull, or crampy. Pain may also spread to the shoulder if bleeding into the abdomen has occurred. Severe bleeding may result in a fast heart rate, fainting, or shock. With very rare exceptions the fetus is unable to survive.

The Dalkon Shield was a contraceptive intrauterine device (IUD) developed by the Dalkon Corporation and marketed by the A.H. Robins Company. The Dalkon Shield was found to cause severe injury to a disproportionately large percentage of women, which eventually led to numerous lawsuits, in which juries awarded millions of dollars in compensatory and punitive damages.
Heavy menstrual bleeding, previously known as menorrhagia, is a menstrual period with excessively heavy flow. It is a type of abnormal uterine bleeding (AUB).

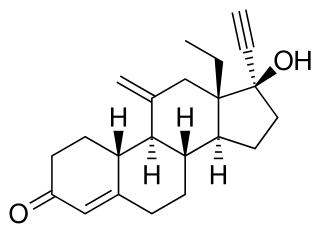
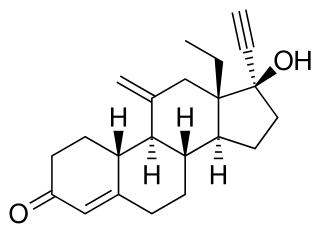
Levonorgestrel is a hormonal medication which is used in a number of birth control methods. It is combined with an estrogen to make combination birth control pills. As an emergency birth control, sold under the brand name Plan B among others, it is useful within 72 hours. This should not be confused with EllaOne which can be effective within 120 hours of unprotected sex. The more time that has passed since sex, the less effective the medication becomes, and it does not work after pregnancy (implantation) has occurred. It decreases the chances of pregnancy by 57 to 93%. In an intrauterine device (IUD), such as Mirena among others, it is effective for the long-term prevention of pregnancy. A levonorgestrel-releasing implant is also available in some countries.

Asherman's syndrome (AS), is an acquired uterine condition that occurs when scar tissue (adhesions) form inside the uterus and/or the cervix. It is characterized by variable scarring inside the uterine cavity, where in many cases the front and back walls of the uterus stick to one another. AS can be the cause of menstrual disturbances, infertility, and placental abnormalities. Although the first case of intrauterine adhesion was published in 1894 by Heinrich Fritsch, it was only after 54 years that a full description of Asherman syndrome was carried out by Joseph Asherman. A number of other terms have been used to describe the condition and related conditions including: uterine/cervical atresia, traumatic uterine atrophy, sclerotic endometrium, and endometrial sclerosis.

Hysteroscopy is the inspection of the uterine cavity by endoscopy with access through the cervix. It allows for the diagnosis of intrauterine pathology and serves as a method for surgical intervention.
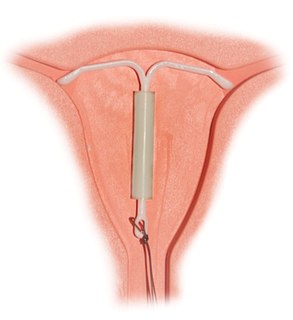
Intrauterine system (IUS) with progestogen, sold under the brand name Mirena among others, is an intrauterine device that releases the hormone levonorgestrel into the uterus. It is used for birth control, heavy menstrual periods, and to prevent excessive build of the lining of the uterus in those on estrogen replacement therapy. It is one of the most effective forms of birth control with a one-year failure rate around 0.2%. The device is placed in the uterus and lasts three to seven years. Fertility often returns quickly following removal.
Etonogestrel is a medication which is used as a means of birth control for women. It is available as an implant placed under the skin of the upper arm under the brand names Nexplanon and Implanon, and in combination with ethinylestradiol, an estrogen, as a vaginal ring under the brand names NuvaRing and Circlet. Etonogestrel is effective as a means of birth control within 8 hours of insertion and lasts at least three or four years with some data showing effectiveness for five years. Following removal, fertility quickly returns.

Controversy over the beginning of pregnancy occurs in different contexts, particularly as it is discussed within the abortion debate in the United States. Because an abortion is defined as ending an established pregnancy, rather than as destroying a fertilized egg, depending on when pregnancy is considered to begin, some methods of birth control as well as some methods of infertility treatment might be classified as causing abortions.

A bicornuate uterus or bicornate uterus, is a type of mullerian anomaly in the human uterus, where there is a deep indentation at the fundus (top) of the uterus.

There are many methods of birth control, they vary in what is required of the user, side effects, and effectiveness. It is also important to note that not every method of birth control is ideal for each user. Outlined here are the different types of barrier methods, hormonal methods, various methods including spermicides, emergency contraceptives, and surgical methods.
Long-acting reversible contraceptives (LARC) are methods of birth control that provide effective contraception for an extended period without requiring user action. They include injections, intrauterine devices (IUDs), and subdermal contraceptive implants. They are the most effective reversible methods of contraception because their efficacy is not reliant on patient compliance. The 'typical use' failure rates of IUDs and implants, at less than 1% per year, are about the same as 'perfect use' failure rates.

A contraceptive implant is an implantable medical device used for the purpose of birth control. The implant may depend on the timed release of hormones to hinder ovulation or sperm development, the ability of copper to act as a natural spermicide within the uterus, or it may work using a non-hormonal, physical blocking mechanism. As with other contraceptives, a contraceptive implant is designed to prevent pregnancy, but it does not protect against sexually transmitted infections.

Birth control, also known as contraception, anticonception, and fertility control, is a method or device used to prevent pregnancy. Birth control has been used since ancient times, but effective and safe methods of birth control only became available in the 20th century. Planning, making available, and using birth control is called family planning. Some cultures limit or discourage access to birth control because they consider it to be morally, religiously, or politically undesirable.

An intrauterine device (IUD), also known as intrauterine contraceptive device or coil, is a small, often T-shaped birth control device that is inserted into the uterus to prevent pregnancy. IUDs are one form of long-acting reversible birth control (LARC). One study found that female family planning providers choose LARC methods more often (41.7%) than the general public (12.1%). Among birth control methods, IUDs, along with other contraceptive implants, result in the greatest satisfaction among users.
Ovarian pregnancy refers to an ectopic pregnancy that is located in the ovary. Typically the egg cell is not released or picked up at ovulation, but fertilized within the ovary where the pregnancy implants. Such a pregnancy usually does not proceed past the first four weeks of pregnancy. An untreated ovarian pregnancy causes potentially fatal intra-abdominal bleeding and thus may become a medical emergency.
Uterine balloon tamponade (UBT) is a non-surgical method of treating refractory postpartum hemorrhage. Once postpartum hemorrhage has been identified and medical management given, UBT may be employed to tamponade uterine bleeding without the need to pursue operative intervention. Numerous studies have supported the efficacy of UBT as a means of managing refractory postpartum hemorrhage. The International Federation of Gynecology and Obstetrics (FIGO) and the World Health Organization (WHO) recommend UBT as second-line treatment for severe postpartum hemorrhage.