Related Research Articles

Eye surgery, also known as ophthalmic surgery or ocular surgery, is surgery performed on the eye or its adnexa. Eye surgery is part of ophthalmology and is performed by an ophthalmologist or eye surgeon. The eye is a fragile organ, and requires due care before, during, and after a surgical procedure to minimize or prevent further damage. An eye surgeon is responsible for selecting the appropriate surgical procedure for the patient, and for taking the necessary safety precautions. Mentions of eye surgery can be found in several ancient texts dating back as early as 1800 BC, with cataract treatment starting in the fifth century BC. It continues to be a widely practiced class of surgery, with various techniques having been developed for treating eye problems.

The corneal endothelium is a single layer of endothelial cells on the inner surface of the cornea. It faces the chamber formed between the cornea and the iris.

Corneal transplantation, also known as corneal grafting, is a surgical procedure where a damaged or diseased cornea is replaced by donated corneal tissue. When the entire cornea is replaced it is known as penetrating keratoplasty and when only part of the cornea is replaced it is known as lamellar keratoplasty. Keratoplasty simply means surgery to the cornea. The graft is taken from a recently deceased individual with no known diseases or other factors that may affect the chance of survival of the donated tissue or the health of the recipient.

Fuchs dystrophy, also referred to as Fuchs endothelial corneal dystrophy (FECD) and Fuchs endothelial dystrophy (FED), is a slowly progressing corneal dystrophy that usually affects both eyes and is slightly more common in women than in men. Although early signs of Fuchs dystrophy are sometimes seen in people in their 30s and 40s, the disease rarely affects vision until people reach their 50s and 60s.

Eduard Konrad Zirm was an Austrian ophthalmologist who performed the first successful human full-thickness corneal transplant on 7 December 1905.
Eye banks recover, prepare and deliver donated eyes for cornea transplants and research. The first successful cornea transplant was performed in 1905 and the first eye bank was founded in 1944. Currently, in the United States, eye banks provide tissue for over 80,000 cornea transplants each year to treat conditions such as keratoconus and corneal scarring. In some cases, the white of the eye (sclera) is used to surgically repair recipient eyes. Unlike other organs and tissues, corneas are in adequate supply for transplants in the United States, and excess tissue is exported internationally, where there are shortages in many countries, due to greater demand and a less-developed eye banking infrastructure.

Descemet's membrane is the basement membrane that lies between the corneal proper substance, also called stroma, and the endothelial layer of the cornea. It is composed of different kinds of collagen than the stroma. The endothelial layer is located at the posterior of the cornea. Descemet's membrane, as the basement membrane for the endothelial layer, is secreted by the single layer of squamous epithelial cells that compose the endothelial layer of the cornea.
Iridocorneal endothelial (ICE) syndromes are a spectrum of diseases characterized by slowly progressive abnormalities of the corneal endothelium and features including corneal edema, iris distortion, and secondary angle-closure glaucoma. ICE syndromes are predominantly unilateral and nonhereditary. The condition occurs in predominantly middle-aged women.Iridocorneal Endothelial (ICE) syndrome presents a unique set of challenges for both patients and ophthalmologists, and effective treatment of this group of rare ocular diseases requires a combination of diagnostic and therapeutic complexity. It's important to understand.
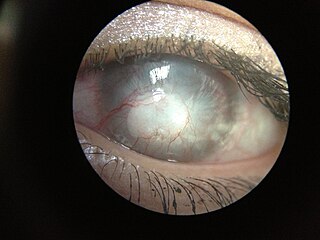
Corneal neovascularization (CNV) is the in-growth of new blood vessels from the pericorneal plexus into avascular corneal tissue as a result of oxygen deprivation. Maintaining avascularity of the corneal stroma is an important aspect of healthy corneal physiology as it is required for corneal transparency and optimal vision. A decrease in corneal transparency causes visual acuity deterioration. Corneal tissue is avascular in nature and the presence of vascularization, which can be deep or superficial, is always pathologically related.

Pellucid marginal degeneration (PMD) is a degenerative corneal condition, often confused with keratoconus. It typically presents with painless vision loss affecting both eyes. Rarely, it may cause acute vision loss with severe pain due to perforation of the cornea. It is typically characterized by a clear, bilateral thinning (ectasia) in the inferior and peripheral region of the cornea, although some cases affect only one eye. The cause of the disease remains unclear.

Bullous keratopathy, also known as pseudophakic bullous keratopathy (PBK), is a pathological condition in which small vesicles, or bullae, are formed in the cornea due to endothelial dysfunction.
Bascom Palmer Eye Institute is the University of Miami School of Medicine's ophthalmic care, research, and education center. The institute is based in the Health District of Miami, Florida, and has been ranked consistently as the best eye hospital and vision research center in the nation.
Dua's layer, according to a 2013 paper by Harminder Singh Dua's group at the University of Nottingham, is a layer of the cornea that had not been detected previously. It is hypothetically 15 micrometres thick, the fourth caudal layer, and located between the corneal stroma and Descemet's membrane. Despite its thinness, the layer is very strong and impervious to air. It is strong enough to withstand up to 2 bars of pressure. While some scientists welcomed the announcement, other scientists cautioned that time was needed for other researchers to confirm the discovery and its significance. Others have met the claim "with incredulity".

Reza Dana is the Claes H. Dohlman Professor of Ophthalmology, senior scientist and W. Clement Stone Clinical Research Scholar at Massachusetts Eye and Ear, Harvard Medical School, and director of the Harvard-Vision Clinical Scientist Development Program.
The Universitäts-Augenklinik Düsseldorf is the department of Ophthalmology of the University Hospital of Düsseldorf in Germany. It is an internationally renown centre for corneal transplantation, ocular surface disease and management of associated disorders ranging from Glaucoma to oculoplastic surgery. Further subspecialist expertise is established for the diagnosis and surgical and medical treatment of vitreoretinal and macular disorders as well as strabismus.
Pre Descemet's endothelial keratoplasty (PDEK) is a kind of endothelial keratoplasty, where the pre descemet's layer (PDL) along with descemet's membrane (DM) and endothelium is transplanted. Conventionally in a corneal transplantation, doctors use a whole cornea or parts of the five layers of the cornea to perform correction surgeries. In May 2013, Dr Harminder Dua discovered a sixth layer between the stroma and the descemet membrane which was named after him as the Dua's layer. In the PDEK technique, doctors take the innermost two layers of the cornea, along with the Dua's layer and graft it in the patient's eye.
ProfessorKeryn Anne Williams is an Australian medical scientist who works in the field of ophthalmology. She was a Principal Research Fellow in the School of Medicine at Flinders University. Her research interests include clinical and experimental corneal transplantation, ocular inflammation, ocular immunology and eye banking.

A corneal button is a replacement cornea to be transplanted in the place of a damaged, diseased or opacified cornea, normally approximately 8.5–9.0mm in diameter. It is used in a corneal transplantation procedure whereby the whole, or part, of a cornea is replaced. The donor tissue can now be held for days to even weeks of the donor's death and is normally a small, rounded shape. The main use of the corneal button is during procedures where the entirety of the cornea needs to be replaced, also known as penetrating keratoplasty.

Corneal opacification is a term used when the human cornea loses its transparency. The term corneal opacity is used particularly for the loss of transparency of cornea due to scarring. Transparency of the cornea is dependent on the uniform diameter and the regular spacing and arrangement of the collagen fibrils within the stroma. Alterations in the spacing of collagen fibrils in a variety of conditions including corneal edema, scars, and macular corneal dystrophy is clinically manifested as corneal opacity. The term corneal blindness is commonly used to describe blindness due to corneal opacity.

Peter Szurman is a German ophthalmologist, scientist, and professor of ophthalmology in Sulzbach/Saar.
References
- 1 2 3 "Legacy Devers Eye Institute". Oregon Lions Sight and Hearing Foundation. Retrieved 23 January 2016.
- ↑ "Devers Memorial Eye Clinic". Legacy Health. Retrieved 23 January 2016.
- ↑ L. Deng; S. Demirel; S.K. Gardiner (June 2014). "Reducing variability in visual field assessment through filtering that combines structural and functional information". Invest. Ophthalmol. Vis. Sci. 13: 13813.
- ↑ Fernandez, MM; Afshari, NA (2010). "Endothelial Keratoplasty: From DLEK to DMEK". Middle East Afr J Ophthalmol. 17 (1): 5–8. doi: 10.4103/0974-9233.61210 (inactive 31 January 2024). PMC 2880365 . PMID 20543930.
{{cite journal}}: CS1 maint: DOI inactive as of January 2024 (link) (mentioning the work of Devers ophthalmologist Mark Terry) - ↑ "DSEK Pearls from Mark Terry, M.D." ophthalmologyweb.com. 28 May 2008.
- ↑ Rumler, J. (January 2014). "Renowned Devers Eye Institute Expands". The Scribe. Portland, Oregon: Medical Society of Metropolitan Portland. 32 (1): 1.
- ↑ "Richard "Dick" Chenoweth, MD". visiongift.org.
- ↑ "Richard Chenoweth Obituary". oregonlive.com.
- ↑ "Schnitzer/Novack Foundation Donates $2 Million to Portland's Two Nationally Known Eye Care Institutes".
- ↑ Rumler, J. (March 2015). "Devers researchers in national spotlight". The Scribe. Portland, Oregon: Medical Society of Metropolitan Portland. 33 (3): 1.
- ↑ "Editors biographies". American Journal of Ophthalmology. Retrieved 19 March 2016.
- ↑ "R. Townley Paton Award". Eye Bank Association of America. Retrieved 19 March 2016.
- ↑ "UAB - SOM - Dept of Ophthalmology - J. Crawford Downs, Ph.D." uab.edu. Archived from the original on 2016-02-07. Retrieved 2016-02-06.
- ↑ "Laboratory of Ocular Biomechanics". ocularbiomechanics.com.
- ↑ "Baylor College of Medicine Appoints Dr. Timothy Stout Chair Of Ophthalmology". BioNews Texas.
- ↑ Samanlego, Chiles Aedam R. (29 April 2014). "New therapeutic dimensions in corneal transplantation". Eyeworld Daily News. p. 20. Retrieved 6 February 2016.
- ↑ Boyle, Erin L. (February 2014). "DMEK experts offer pearls, pitfalls for performing procedure". Eyeworld. Retrieved 6 February 2016.
- ↑ "Department of Ophthalmology and Visual Science, University of Chicago".
- ↑ "Cornea Clinic".