| Low pressure hydrocephalus | |
|---|---|
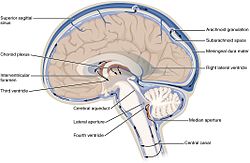 | |
| Ventricles position | |
| Specialty | Neurology |
Low-pressure hydrocephalus (LPH) is a condition whereby ventricles are enlarged and the individual experiences severe dementia, inability to walk or gait disturbance, and incontinence despite very low intracranial pressure (ICP). [1]
LPH is considered a more acute variant of normal pressure hydrocephalus. Without timely diagnosis, patients may remain in a persistent low-pressure hydrocephalic state (LPHS). Standard shunt revisions, even with low-pressure settings, may be ineffective because ICP does not rise sufficiently to allow adequate cerebrospinal fluid (CSF) drainage. In such cases, the shunt remains patent but functionally ineffective. Chronic infarcts along the corona radiata can occur due to parenchymal stretching as the ventricles enlarge.
Reported causes of LPH include head trauma, tumours, intracranial haemorrhage, meningitis, whole-brain radiotherapy, and other conditions that alter brain parenchymal compliance. One treatment approach for LPHS is the use of an external ventricular drain (EVD) set at negative pressures. Pang and Altschuler et al. have described controlled, steady, negative-pressure siphoning with EVD, monitored via serial partial computed tomography (CT) scans, as a safe and effective means of reducing ventricular size and restoring the brain mantle. [2] They caution against rapid adjustments to EVD pressure, which can destabilise the ventricles and increase risk. Their recommended management sequence involves ventricular size reduction, stabilisation and, finally, shunt placement. Deviation from this sequence can result in a patent but ineffective shunt. Mismanagement of EVD therapy may cause permanent neurological complications. [2]