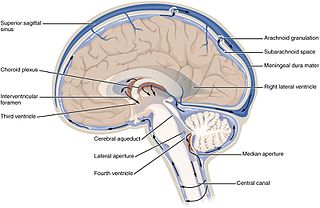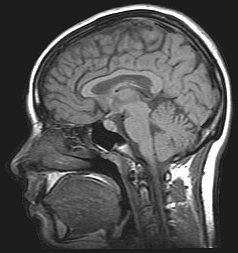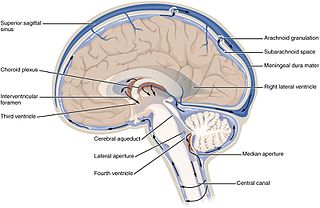
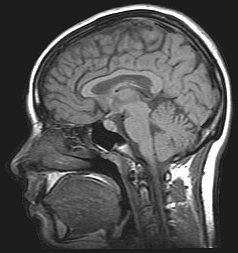
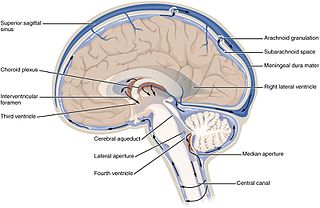
Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.
Idiopathic intracranial hypertension (IIH), previously known as pseudotumor cerebri and benign intracranial hypertension, is a condition characterized by increased intracranial pressure without a detectable cause. The main symptoms are headache, vision problems, ringing in the ears, and shoulder pain. Complications may include vision loss.

Hydrocephalus is a condition in which an accumulation of cerebrospinal fluid (CSF) occurs within the brain. This typically causes increased pressure inside the skull. Older people may have headaches, double vision, poor balance, urinary incontinence, personality changes, or mental impairment. In babies, it may be seen as a rapid increase in head size. Other symptoms may include vomiting, sleepiness, seizures, and downward pointing of the eyes.

Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and at rest, is normally 7–15 mmHg for a supine adult. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.

Subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space—the area between the arachnoid membrane and the pia mater surrounding the brain. Symptoms may include a severe headache of rapid onset, vomiting, decreased level of consciousness, fever, weakness, numbness, and sometimes seizures. Neck stiffness or neck pain are also relatively common. In about a quarter of people a small bleed with resolving symptoms occurs within a month of a larger bleed.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds. More often than not it ends in death.
Normal-pressure hydrocephalus (NPH), also called malresorptive hydrocephalus, is a form of communicating hydrocephalus in which excess cerebrospinal fluid (CSF) occurs in the ventricles, and with normal or slightly elevated cerebrospinal fluid pressure. As the fluid builds up, it causes the ventricles to enlarge and the pressure inside the head to increase, compressing surrounding brain tissue and leading to neurological complications. The disease presents in a classic triad of symptoms, which are memory impairment, urinary frequency, and balance problems/gait deviations. The disease was first described by Salomón Hakim and Adams in 1965.

Intracerebral hemorrhage (ICH), also known as hemorrhagic stroke, is a sudden bleeding into the tissues of the brain, into its ventricles, or into both. An ICH is a type of bleeding within the skull and one kind of stroke. Symptoms can vary dramatically depending on the severity, acuity, and location (anatomically) but can include headache, one-sided weakness, numbness, tingling, or paralysis, speech problems, vision or hearing problems, memory loss, attention problems, coordination problems, balance problems, dizziness or lightheadedness or vertigo, nausea/vomiting, seizures, decreased level of consciousness or total loss of consciousness, neck stiffness, and fever.

Ventriculitis is the inflammation of the ventricles in the brain. The ventricles are responsible for containing and circulating cerebrospinal fluid throughout the brain. Ventriculitis is caused by infection of the ventricles, leading to swelling and inflammation. This is especially prevalent in patients with external ventricular drains and intraventricular stents. Ventriculitis can cause a wide variety of short-term symptoms and long-term side effects ranging from headaches and dizziness to unconsciousness and death if not treated early. It is treated with some appropriate combination of antibiotics in order to rid the patient of the underlying infection. Much of the current research involving ventriculitis focuses specifically around defining the disease and what causes it. This will allow for much more advancement in the subject. There is also a lot of attention being paid to possible treatments and prevention methods to help make this disease even less prevalent and dangerous.

A subdural hygroma (SDG) is a collection of cerebrospinal fluid (CSF), without blood, located under the dural membrane of the brain. Most subdural hygromas are believed to be derived from chronic subdural hematomas. They are commonly seen in elderly people after minor trauma but can also be seen in children following infection or trauma. One of the common causes of subdural hygroma is a sudden decrease in pressure as a result of placing a ventricular shunt. This can lead to leakage of CSF into the subdural space especially in cases with moderate to severe brain atrophy. In these cases the symptoms such as mild fever, headache, drowsiness and confusion can be seen, which are relieved by draining this subdural fluid.

A colloid cyst is a non-malignant tumor in the brain. It consists of a gelatinous material contained within a membrane of epithelial tissue. It is almost always found just posterior to the foramen of Monro in the anterior aspect of the third ventricle, originating from the roof of the ventricle. Because of its location, it can cause obstructive hydrocephalus and increased intracranial pressure. Colloid cysts represent 0.5–1.0% of intracranial tumors.
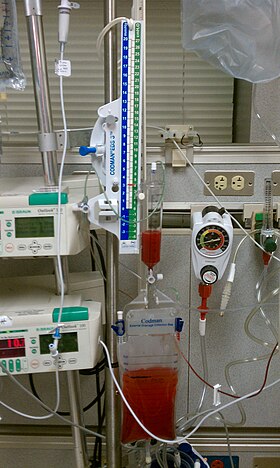
Ventriculostomy is a neurosurgical procedure that involves creating a hole (stoma) within a cerebral ventricle for drainage. It is most commonly performed on those with hydrocephalus. It is done by surgically penetrating the skull, dura mater, and brain such that the ventricular system ventricle of the brain is accessed. When catheter drainage is temporary, it is commonly referred to as an external ventricular drain (EVD). When catheter drainage is permanent, it is usually referred to as a shunt. There are many catheter-based ventricular shunts that are named for where they terminate, for example, a ventriculi-peritoneal shunt terminates in the peritoneal cavity, a ventriculoarterial shunt terminates within the atrium of the heart, etc. The most common entry point on the skull is called Kocher's point, which is measured 11 cm posterior to the nasion and 3 cm lateral to midline. EVD ventriculostomy is done primarily to monitor the intracranial pressure as well as to drain cerebrospinal fluid (CSF), primarily, or blood to relieve pressure from the central nervous system (CNS).

A cerebral shunt is a device permanently implanted inside the head and body to drain excess fluid away from the brain. They are commonly used to treat hydrocephalus, the swelling of the brain due to excess buildup of cerebrospinal fluid (CSF). If left unchecked, the excess CSF can lead to an increase in intracranial pressure (ICP), which can cause intracranial hematoma, cerebral edema, crushed brain tissue or herniation. The drainage provided by a shunt can alleviate or prevent these problems in patients with hydrocephalus or related diseases.

Intraventricular hemorrhage (IVH), also known as intraventricular bleeding, is a bleeding into the brain's ventricular system, where the cerebrospinal fluid is produced and circulates through towards the subarachnoid space. It can result from physical trauma or from hemorrhagic stroke.

Neurocritical care is a medical field that treats life-threatening diseases of the nervous system and identifies, prevents, and treats secondary brain injury.
Endoscopic third ventriculostomy (ETV) is a surgical procedure for treatment of hydrocephalus in which an opening is created in the floor of the third ventricle using an endoscope placed within the ventricular system through a burr hole. This allows the cerebrospinal fluid to flow directly to the basal cisterns, bypassing the obstruction. Specifically, the opening is created in the translucent tuber cinereum on the third ventricular floor.
A lumbar–peritoneal shunt is a technique to channelise the cerebrospinal fluid (CSF) from the lumbar thecal sac into the peritoneal cavity.
Low-pressure hydrocephalus (LPH) is a condition whereby ventricles are enlarged and the individual experiences severe dementia, inability to walk, and incontinence – despite very low intracranial pressure (ICP).
The monitoring of intracranial pressure (ICP) is used in the treatment of a number of neurological conditions ranging from severe traumatic brain injury to stroke and brain bleeds. This process is called intracranial pressure monitoring. Monitoring is important as persistent increases in ICP is associated with worse prognosis in brain injuries due to decreased oxygen delivery to the injured area and risk of brain herniation.

Aqueductal stenosis is a narrowing of the aqueduct of Sylvius which blocks the flow of cerebrospinal fluid (CSF) in the ventricular system. Blockage of the aqueduct can lead to hydrocephalus, specifically as a common cause of congenital and/or obstructive hydrocephalus.