Brain abscess is an abscess within the brain tissue caused by inflammation and collection of infected material coming from local or remote infectious sources. The infection may also be introduced through a skull fracture following a head trauma or surgical procedures. Brain abscess is usually associated with congenital heart disease in young children. It may occur at any age but is most frequent in the third decade of life.
Idiopathic intracranial hypertension (IIH), previously known as pseudotumor cerebri and benign intracranial hypertension, is a condition characterized by increased intracranial pressure without a detectable cause. The main symptoms are headache, vision problems, ringing in the ears, and shoulder pain. Complications may include vision loss.

A brain tumor occurs when abnormal cells form within the brain. There are two main types of tumors: malignant (cancerous) tumors and benign (non-cancerous) tumors. These can be further classified as primary tumors, which start within the brain, and secondary tumors, which most commonly have spread from tumors located outside the brain, known as brain metastasis tumors. All types of brain tumors may produce symptoms that vary depending on the size of the tumor and the part of the brain that is involved. Where symptoms exist, they may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking, with sensations, or unconsciousness.

A head injury is any injury that results in trauma to the skull or brain. The terms traumatic brain injury and head injury are often used interchangeably in the medical literature. Because head injuries cover such a broad scope of injuries, there are many causes—including accidents, falls, physical assault, or traffic accidents—that can cause head injuries.

Headache, also known as cephalalgia, is the symptom of pain in the face, head, or neck. It can occur as a migraine, tension-type headache, or cluster headache. There is an increased risk of depression in those with severe headaches.

Cerebral edema is excess accumulation of fluid (edema) in the intracellular or extracellular spaces of the brain. This typically causes impaired nerve function, increased pressure within the skull, and can eventually lead to direct compression of brain tissue and blood vessels. Symptoms vary based on the location and extent of edema and generally include headaches, nausea, vomiting, seizures, drowsiness, visual disturbances, dizziness, and in severe cases, death.

Pneumoencephalography was a common medical procedure in which most of the cerebrospinal fluid (CSF) was drained from around the brain by means of a lumbar puncture and replaced with air, oxygen, or helium to allow the structure of the brain to show up more clearly on an X-ray image. It was derived from ventriculography, an earlier and more primitive method in which the air is injected through holes drilled in the skull.

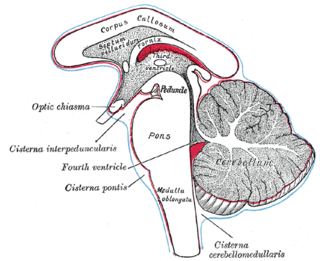
Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and at rest, is normally 7–15 mmHg for a supine adult. This equals to 9–20 cmH2O, which is a common scale used in lumbar punctures. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.

A subdural hematoma (SDH) is a type of bleeding in which a collection of blood—usually but not always associated with a traumatic brain injury—gathers between the inner layer of the dura mater and the arachnoid mater of the meninges surrounding the brain. It usually results from tears in bridging veins that cross the subdural space.

Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds.

Epidural hematoma is when bleeding occurs between the tough outer membrane covering the brain and the skull. When this condition occurs in the spinal canal, it is known as a spinal epidural hematoma.
Normal pressure hydrocephalus (NPH), also called malresorptive hydrocephalus, is a form of communicating hydrocephalus in which excess cerebrospinal fluid (CSF) builds up in the ventricles, leading to normal or slightly elevated cerebrospinal fluid pressure. The fluid build-up causes the ventricles to enlarge and the pressure inside the head to increase, compressing surrounding brain tissue and leading to neurological complications. Although the cause of idiopathicNPH remains unclear, it has been associated with various co-morbidities including hypertension, diabetes mellitus, Alzheimer's disease, and hyperlipidemia. Causes of secondary NPH include trauma, hemorrhage, or infection. The disease presents in a classic triad of symptoms, which are memory impairment, urinary frequency, and balance problems/gait deviations. The disease was first described by Salomón Hakim and Raymond Adams in 1965.
A thunderclap headache is a headache that is severe and has a sudden onset. It is defined as a severe headache that takes seconds to minutes to reach maximum intensity. Although approximately 75% are attributed to "primary" headaches—headache disorder, non-specific headache, idiopathic thunderclap headache, or uncertain headache disorder—the remainder are secondary to other causes, which can include some extremely dangerous acute conditions, as well as infections and other conditions. Usually, further investigations are performed to identify the underlying cause.

Intracerebral hemorrhage (ICH), also known as hemorrhagic stroke, is a sudden bleeding into the tissues of the brain, into its ventricles, or into both. An ICH is a type of bleeding within the skull and one kind of stroke. Symptoms can vary dramatically depending on the severity, acuity, and location (anatomically) but can include headache, one-sided weakness, numbness, tingling, or paralysis, speech problems, vision or hearing problems, memory loss, attention problems, coordination problems, balance problems, dizziness or lightheadedness or vertigo, nausea/vomiting, seizures, decreased level of consciousness or total loss of consciousness, neck stiffness, and fever.

Brain herniation is a potentially deadly side effect of very high pressure within the skull that occurs when a part of the brain is squeezed across structures within the skull. The brain can shift across such structures as the falx cerebri, the tentorium cerebelli, and even through the foramen magnum. Herniation can be caused by a number of factors that cause a mass effect and increase intracranial pressure (ICP): these include traumatic brain injury, intracranial hemorrhage, or brain tumor.
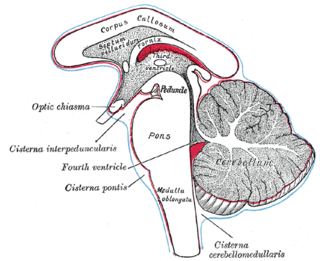
Duret haemorrhages are small linear areas of bleeding in the midbrain and upper pons of the brainstem. They are caused by a traumatic downward displacement of the brainstem.

A subdural hygroma (SDG) is a collection of cerebrospinal fluid (CSF), without blood, located under the dural membrane of the brain. Most subdural hygromas are believed to be derived from chronic subdural hematomas. They are commonly seen in elderly people after minor trauma but can also be seen in children following infection or trauma. One of the common causes of subdural hygroma is a sudden decrease in pressure as a result of placing a ventricular shunt. This can lead to leakage of CSF into the subdural space especially in cases with moderate to severe brain atrophy. In these cases the symptoms such as mild fever, headache, drowsiness and confusion can be seen, which are relieved by draining this subdural fluid.
Kernohan's notch is a cerebral peduncle indentation associated with some forms of transtentorial herniation. It is a secondary condition caused by a primary injury on the opposite hemisphere of the brain. Kernohan's notch is an ipsilateral condition, in that a left-sided primary lesion evokes motor impairment in the left side of the body and a right-sided primary injury evokes motor impairment in the right side of the body. The seriousness of Kernohan's notch varies depending on the primary problem causing it, which may range from benign brain tumors to advanced subdural hematoma.

Midline shift is a shift of the brain past its center line. The sign may be evident on neuroimaging such as CT scanning. The sign is considered ominous because it is commonly associated with a distortion of the brain stem that can cause serious dysfunction evidenced by abnormal posturing and failure of the pupils to constrict in response to light. Midline shift is often associated with high intracranial pressure (ICP), which can be deadly. In fact, midline shift is a measure of ICP; presence of the former is an indication of the latter. Presence of midline shift is an indication for neurosurgeons to take measures to monitor and control ICP. Immediate surgery may be indicated when there is a midline shift of over 5 mm. The sign can be caused by conditions including traumatic brain injury, stroke, hematoma, or birth deformity that leads to a raised intracranial pressure.
Adrenal hemorrhage (AH) is acute blood loss from a ruptured vessel of the adrenal glands above the kidneys.