Related Research Articles

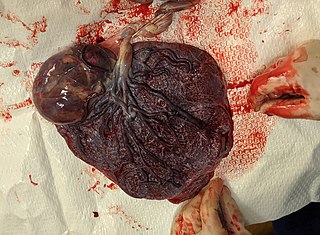
The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate maternal and fetal circulations, and is an important endocrine organ, producing hormones that regulate both maternal and fetal physiology during pregnancy. The placenta connects to the fetus via the umbilical cord, and on the opposite aspect to the maternal uterus in a species-dependent manner. In humans, a thin layer of maternal decidual (endometrial) tissue comes away with the placenta when it is expelled from the uterus following birth. Placentas are a defining characteristic of placental mammals, but are also found in marsupials and some non-mammals with varying levels of development.

The chorion is the outermost fetal membrane around the embryo in mammals, birds and reptiles (amniotes). It develops from an outer fold on the surface of the yolk sac, which lies outside the zona pellucida, known as the vitelline membrane in other animals. In insects, it is developed by the follicle cells while the egg is in the ovary. Some mollusks also have chorions as part of their eggs. For example, fragile octopus eggs have only a chorion as their envelope.

The trophoblast is the outer layer of cells of the blastocyst. Trophoblasts are present four days after fertilization in humans. They provide nutrients to the embryo and develop into a large part of the placenta. They form during the first stage of pregnancy and are the first cells to differentiate from the fertilized egg to become extraembryonic structures that do not directly contribute to the embryo. After blastulation, the trophoblast is contiguous with the ectoderm of the embryo and is referred to as the trophectoderm. After the first differentiation, the cells in the human embryo lose their totipotency because they can no longer form a trophoblast. They become pluripotent stem cells.

The decidua is the modified mucosal lining of the uterus that forms every month, in preparation for pregnancy. It is shed off each month when there is no fertilized egg to support. The decidua is under the influence of progesterone. Endometrial cells become highly characteristic. The decidua forms the maternal part of the placenta and remains for the duration of the pregnancy. After birth the decidua is shed together with the placenta.

The syncytiotrophoblast is the epithelial covering of the highly vascular embryonic placental villi, which invades the wall of the uterus to establish nutrient circulation between the embryo and the mother. It is a multinucleate, terminally differentiated syncytium, extending to 13 cm.

Intrauterine hypoxia occurs when the fetus is deprived of an adequate supply of oxygen. It may be due to a variety of reasons such as prolapse or occlusion of the umbilical cord, placental infarction, maternal diabetes and maternal smoking. Intrauterine growth restriction may cause or be the result of hypoxia. Intrauterine hypoxia can cause cellular damage that occurs within the central nervous system. This results in an increased mortality rate, including an increased risk of sudden infant death syndrome (SIDS). Oxygen deprivation in the fetus and neonate have been implicated as either a primary or as a contributing risk factor in numerous neurological and neuropsychiatric disorders such as epilepsy, attention deficit hyperactivity disorder, eating disorders and cerebral palsy.

Placenta accreta occurs when all or part of the placenta attaches abnormally to the myometrium. Three grades of abnormal placental attachment are defined according to the depth of attachment and invasion into the muscular layers of the uterus:
- Accreta – chorionic villi attached to the myometrium, rather than being restricted within the decidua basalis.
- Increta – chorionic villi invaded into the myometrium.
- Percreta – chorionic villi invaded through the perimetrium.

Placentation is the formation, type and structure, or arrangement of the placenta. The function of placentation is to transfer nutrients, respiratory gases, and water from maternal tissue to a growing embryo, and in some instances to remove waste from the embryo. Placentation is best known in live-bearing mammals (Theria), but also occurs in some fish, reptiles, amphibians, a diversity of invertebrates, and flowering plants. In vertebrates, placentas have evolved more than 100 times independently, with the majority of these instances occurring in squamate reptiles.
Hofbauer cells are oval eosinophilic histiocytes with granules and vacuoles found in the placenta, which are of mesenchymal origin, in mesoderm of the chorionic villi, particularly numerous in early pregnancy.
Placental insufficiency or utero-placental insufficiency is the failure of the placenta to deliver sufficient nutrients to the fetus during pregnancy, and is often a result of insufficient blood flow to the placenta. The term is also sometimes used to designate late decelerations of fetal heart rate as measured by cardiotocography or an NST, even if there is no other evidence of reduced blood flow to the placenta, normal uterine blood flow rate being 600mL/min.

Uterine glands or endometrial glands are tubular glands, lined by a simple columnar epithelium, found in the functional layer of the endometrium that lines the uterus. Their appearance varies during the menstrual cycle. During the proliferative phase, uterine glands appear long due to estrogen secretion by the ovaries. During the secretory phase, the uterine glands become very coiled with wide lumens and produce a glycogen-rich secretion known as histotroph or uterine milk. This change corresponds with an increase in blood flow to spiral arteries due to increased progesterone secretion from the corpus luteum. During the pre-menstrual phase, progesterone secretion decreases as the corpus luteum degenerates, which results in decreased blood flow to the spiral arteries. The functional layer of the uterus containing the glands becomes necrotic, and eventually sloughs off during the menstrual phase of the cycle.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.

A placental disease is any disease, disorder, or pathology of the placenta.

Placentitis is an inflammation of the placenta. The main forms of placentitis are:

The fetal membranes are the four extraembryonic membranes, associated with the developing embryo, and fetus in humans and other mammals. They are the amnion, chorion, allantois, and yolk sac. The amnion and the chorion are the chorioamniotic membranes that make up the amniotic sac which surrounds and protects the embryo. The fetal membranes are four of six accessory organs developed by the conceptus that are not part of the embryo itself, the other two are the placenta, and the umbilical cord.

Circumvallate placenta is a rare condition affecting about 1-2% of pregnancies, in which the amnion and chorion fetal membranes essentially "double back" on the fetal side around the edges of the placenta. After delivery, a circumvallate placenta has a thick ring of membranes on its fetal surface. Circumvallate placenta is a placental morphological abnormality associated with increased fetal morbidity and mortality due to the restricted availability of nutrients and oxygen to the developing fetus.
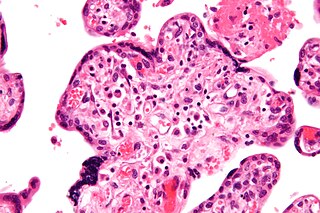
Villitis of unknown etiology (VUE), also known as chronic villitis, is a placental injury. VUE is an inflammatory condition involving the chorionic villi. VUE is a recurrent condition and can be associated with intrauterine growth restriction (IUGR). IUGR involves the poor growth of the foetus, stillbirth, miscarriage, and premature delivery. VUE recurs in about 1/3 of subsequent pregnancies.

A placental infarction results from the interruption of blood supply to a part of the placenta, causing its cells to die.
Chorioangioma, or chorangioma, is a benign tumor of placenta. It is a hamartoma-like growth in the placenta consisting of blood vessels, and is seen in approximately 0.5 to 1% pregnancies. It is mostly diagnosed ultrasonically in the second trimester of pregnancy. Large chorioangiomas are known to cause complications in pregnancy, while the smaller ones are asymptomatic.
Breus' mole is a massive, subchorionic, tuberous hematoma formed from maternal blood in the uterus during pregnancy. It was first described by Karl Breus in 1892.
References
- 1 2 3 4 5 6 Spinillo, Arsenio; Gardella, Barbara; Muscettola, Giulia; Cesari, Stefania; Fiandrino, Giacomo; Tzialla, Chryssoula (November 2019). "The impact of placental massive perivillous fibrin deposition on neonatal outcome in pregnancies complicated by fetal growth restriction". Placenta. 87: 46–52. doi:10.1016/j.placenta.2019.09.007. PMID 31546153. S2CID 202747162.
- 1 2 Devisme, Louise; Chauvière, Claire; Franquet-Ansart, Hélène; Chudzinski, Anastasia; Stichelbout, Morgane; Houfflin-Debarge, Véronique; Subtil, Damien (April 2017). "Perinatal outcome of placental massive perivillous fibrin deposition: a case-control study". Prenatal Diagnosis. 37 (4): 323–328. doi:10.1002/pd.5013. PMID 28152557. S2CID 12908009.
- 1 2 3 4 5 Faye-Petersen, Ona Marie; Ernst, Linda M. (March 2013). "Maternal Floor Infarction and Massive Perivillous Fibrin Deposition". Surgical Pathology Clinics. 6 (1): 101–14. doi:10.1016/j.path.2012.10.002. PMID 26838705.
- ↑ Taweevisit, Mana; Thawornwong, Nutchanok; Thorner, Paul Scott (2021-01-01). "Massive Perivillous Fibrin Deposition Associated With Placental Syphilis: A Case Report". Pediatric and Developmental Pathology. 24 (1): 43–46. doi:10.1177/1093526620957523. PMID 32951526. S2CID 221826726.
- ↑ Sebire, Neil J; Backos, May; Goldin, Robert D.; Regan, Lesley (May 2002). "Placental massive perivillous fibrin deposition associated with antiphospholipid antibody syndrome". BJOG. 109 (5): 570–3. doi:10.1111/j.1471-0528.2002.00077.x. PMID 12066949. S2CID 33748717.
- ↑ Hung, Noelyn Anne; Jackson, Christopher; Nicholson, Martha; Highton, John (February 2006). "Pregnancy-related poymyositis and massive perivillous fibrin deposition in the placenta: are they pathogenetically related?". Arthritis and Rheumatism. 55 (1): 154–6. doi: 10.1002/art.21710 . PMID 16463429.
- ↑ Gestrich, Catherine K; Zhou, Yi Yuan; Ravishankar, Sanjita (2021-01-01). "Massive Perivillous Fibrin Deposition in Congenital Cytomegalovirus Infection: A Case Report". Pediatric and Developmental Pathology. 24 (1): 47–50. doi:10.1177/1093526620961352. PMID 33104416. S2CID 225083262.
- 1 2 Pathak, Sangeeta; Lees, Christoph C.; Hackett, Gerald; Jessop, Flora; Sebire, Neil J. (December 2011). "Frequency and clinical significance of placental histological lesions in an unselected population at or near term". Virchows Archiv. 459 (6): 565–72. doi:10.1007/s00428-011-1157-z. PMID 22038509. S2CID 26004303.
- ↑ Romero, Roberto; Whitten, Amy; Korzeniewski, Steven J.; Than, Nandor G; Chaemsaithong, Piya; Miranda, Jezid; Dong, Zhong; Hassan, Sonia S.; Chaiworapongsa, Tinnakorn (October 2013). "Maternal Floor Infarction/Massive Perivillous Fibrin Deposition: A Manifestation of Maternal Antifetal Rejection". American Journal of Reproductive Immunology. 70 (4): 285–298. doi:10.1111/aji.12143. ISSN 1046-7408. PMC 4122226 . PMID 23905710.
- 1 2 Katzman, Philip J.; Genest, David R. (2002-03-01). "Maternal floor infarction and massive perivillous fibrin deposition: histological definitions, association with intrauterine fetal growth restriction, and risk of recurrence". Pediatric and Developmental Pathology. 5 (2): 159–64. doi:10.1007/s10024001-0195-y. PMID 11910510. S2CID 43397786.
- 1 2 3 4 Bane, Anita L.; Gillan, J. E. (March 2003). "Massive perivillous fibrinoid causing recurrent placental failure". BJOG. 110 (3): 292–5. doi:10.1016/S1470-0328(03)00919-4. PMID 12628270.
- 1 2 Chaiworapongsa, Tinnakorn; Romero, Roberto; Korzeniewski, Steven J.; Chaemsaithong, Piya; Hernandez-Andrade, Edgar; Segars, James H.; DeCherney, Alan H.; McCoy, M. Cathleen; Kim, Chong Jai; Yeo, Lami; Hassan, Sonia S. (March 2016). "Pravastatin to prevent recurrent fetal death in massive perivillous fibrin deposition of the placenta (MPFD)". The Journal of Maternal-Fetal & Neonatal Medicine. 29 (6): 855–62. doi:10.3109/14767058.2015.1022864. PMC 4710361 . PMID 25893545.