Anti-psychiatry, sometimes spelled antipsychiatry, is a movement based on the view that psychiatric treatment is often more damaging than helpful to patients, highlighting controversies about psychiatry. Objections include the reliability of psychiatric diagnosis, the questionable effectiveness and harm associated with psychiatric medications, the failure of psychiatry to demonstrate any disease treatment mechanism for psychiatric medication effects, and legal concerns about equal human rights and civil freedom being nullified by the presence of diagnosis. Historical critiques of psychiatry came to light after focus on the extreme harms associated with electroconvulsive therapy or insulin shock therapy. The term "anti-psychiatry" is in dispute and often used to dismiss all critics of psychiatry, many of whom agree that a specialized role of helper for people in emotional distress may at times be appropriate, and allow for individual choice around treatment decisions.

Electroconvulsive therapy (ECT) or electroshock therapy (EST) is a psychiatric treatment where a generalized seizure is electrically induced to manage refractory mental disorders. Typically, 70 to 120 volts are applied externally to the patient's head, resulting in approximately 800 milliamperes of direct current passing between the electrodes, for a duration of 100 milliseconds to 6 seconds, either from temple to temple or from front to back of one side of the head. However, only about 1% of the electrical current crosses the bony skull into the brain because skull impedance is about 100 times higher than skin impedance.

An advance healthcare directive, also known as living will, personal directive, advance directive, medical directive or advance decision, is a legal document in which a person specifies what actions should be taken for their health if they are no longer able to make decisions for themselves because of illness or incapacity. In the U.S. it has a legal status in itself, whereas in some countries it is legally persuasive without being a legal document.

The Mental Health Act 1983 is an Act of the Parliament of the United Kingdom. It covers the reception, care and treatment of mentally disordered people, the management of their property and other related matters, forming part of the mental health law for the people in England and Wales. In particular, it provides the legislation by which people diagnosed with a mental disorder can be detained in a hospital or police custody and have their disorder assessed or treated against their wishes, informally known as "sectioning". Its use is reviewed and regulated by the Care Quality Commission. The Act was significantly amended by the Mental Health Act 2007. A white paper proposing changes to the act was published in 2021 following an independent review of the act by Simon Wessely.

Suicide is a crime in some parts of the world. However, while suicide has been decriminalized in many countries, the act is almost universally stigmatized and discouraged. In some contexts, suicide could be utilized as an extreme expression of liberty, as is exemplified by its usage as an expression of devout dissent towards perceived tyranny or injustice which occurred occasionally in cultures such as ancient Rome, medieval Japan, or today's Tibet Autonomous Region.
Involuntary treatment refers to medical treatment undertaken without the consent of the person being treated. Involuntary treatment is permitted by law in some countries when overseen by the judiciary through court orders; other countries defer directly to the medical opinions of doctors.
Suicidal ideation, or suicidal thoughts, is the thought process of having ideas, or ruminations about the possibility of completing suicide. It is not a diagnosis but is a symptom of some mental disorders, use of certain psychoactive drugs, and can also occur in response to adverse life events without the presence of a mental disorder.

The healthcare delivery system of Pakistan is complex because it includes healthcare subsystems by federal governments and provincial governments competing with formal and informal private sector healthcare systems. Healthcare is delivered mainly through vertically managed disease-specific mechanisms. The different institutions that are responsible for this include: provincial and district health departments, parastatal organizations, social security institutions, non-governmental organizations (NGOs) and private sector. The country's health sector is also marked by urban-rural disparities in healthcare delivery and an imbalance in the health workforce, with insufficient health managers, nurses, paramedics and skilled birth attendants in the peripheral areas. Pakistan's gross national income per capita in 2021 was $4,990 and the total expenditure on health per capita in 2021 was Rs 657.2 Billion, constituting 1.4% of the country's GDP. The health care delivery system in Pakistan consists of public and private sectors. Under the constitution, health is primarily responsibility of the provincial government, except in the federally administered areas. Health care delivery has traditionally been jointly administered by the federal and provincial governments with districts mainly responsible for implementation. Service delivery is being organized through preventive, promotive, curative and rehabilitative services. The curative and rehabilitative services are being provided mainly at the secondary and tertiary care facilities. Preventive and promotive services, on the other hand, are mainly provided through various national programs; and community health workers’ interfacing with the communities through primary healthcare facilities and outreach activities. The state provides healthcare through a three-tiered healthcare delivery system and a range of public health interventions. Some government/ semi government organizations like the armed forces, Sui Gas, WAPDA, Railways, Fauji Foundation, Employees Social Security Institution and NUST provide health service to their employees and their dependants through their own system, however, these collectively cover about 10% of the population. The private health sector constitutes a diverse group of doctors, nurses, pharmacists, traditional healers, drug vendors, as well as laboratory technicians, shopkeepers and unqualified practitioners.
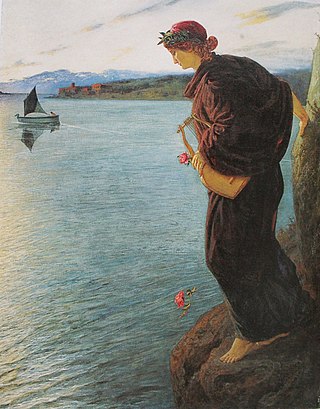
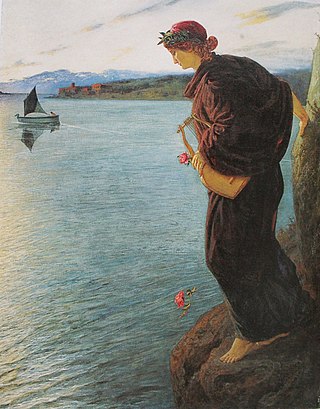
A suicide crisis, suicidal crisis or potential suicide is a situation in which a person is attempting to kill themselves or is seriously contemplating or planning to do so. It is considered by public safety authorities, medical practice, and emergency services to be a medical emergency, requiring immediate suicide intervention and emergency medical treatment. Suicidal presentations occur when an individual faces an emotional, physical, or social problem they feel they cannot overcome and considers suicide to be a solution. Clinicians usually attempt to re-frame suicidal crises, point out that suicide is not a solution and help the individual identify and solve or tolerate the problems.
Services for mental health disorders provide treatment, support, or advocacy to people who have psychiatric illnesses. These may include medical, behavioral, social, and legal services.
A suicide attempt is an act in which an individual tries to kill themselves but survives. Mental health professionals discourage describing suicide attempts as "failed" or "unsuccessful", as doing so may imply that a suicide resulting in death is a successful or desirable outcome.
Section 309 of the Indian Penal Code criminalises attempted suicide as well as suicide assistance.
Psychiatry is, and has historically been, viewed as controversial by those under its care, as well as sociologists and psychiatrists themselves. There are a variety of reasons cited for this controversy, including the subjectivity of diagnosis, the use of diagnosis and treatment for social and political control including detaining citizens and treating them without consent, the side effects of treatments such as electroconvulsive therapy, antipsychotics and historical procedures like the lobotomy and other forms of psychosurgery or insulin shock therapy, and the history of racism within the profession in the United States.

In India, the Mental Health Act was passed on 22 May 1987. The law was described in its opening paragraph as "An Act to consolidate and amend the law relating to the treatment and care of mentally ill persons, to make better provision with respect to their property and affairs and for matters connected therewith or incidental thereto."
The overall prevalence of people with disabilities is 4.52% of the population, i.e., 63.28 million, according to the ICMR's publication from the NFHS-5 survey 2019-21. India is a party to the United Nations Convention on the Rights of Persons with Disabilities. Legislation that affects people with disabilities in India includes the Rights of Persons with Disabilities Act, 2016, the Mental Health Care Act, 2017, the National Trust Act, 1999, and the Rehabilitation Council of India Act, 1992. People with disabilities in India are faced with negative social attitudes in the wider population.
Geriatric psychology is a subfield of psychology that specializes in the mental and physical health of individuals in the later stages of life. These specialized psychologists study a variety of psychological abilities that deplete as aging occurs such as memory, learning capabilities, and coordination. Geriatric psychologists work with elderly clients to conduct the diagnosis, study, and treatment of certain mental illnesses in a variety of workplace settings. Common areas of practice include loneliness in old age, depression, dementia, Alzheimer's disease, vascular dementia, and Parkinson's disease.
Over the past few decades, mental health has become an increasingly serious issue in health in South Korea. A 2021 survey conducted by the Ministry of Health and Welfare found that 32.7% of males and 22.9% of females in South Korea developed symptoms of mental illness at least one time in their lives. Suicide in South Korea is the most frequent cause of death for people aged 9 to 24. Mental health issues are most common among the elderly and adolescents.

Mental healthcare in India is a right secured to every person in the country by law. Indian mental health legislation, as per a 2017 study, meets 68% (119/175) of the World Health Organization (WHO) standards laid down in the WHO Checklist of Mental Health Legislation. However, human resources and expertise in the field of mental health in India is significantly low when compared to the population of the country. The allocation of the national healthcare budget to mental health is also low, standing at 0.16%. India's mental health policy was released in 2014.

Keshav Desiraju was an Indian bureaucrat who served as the union health secretary of the country. He was known for his contributions to mental health and community healthcare and was the architect of the country's Mental Healthcare Act of 2017.
Suicide prevention and intervention efforts in India are in the nascent stage. According to the World Health Organization (WHO), suicide in India is a serious public health issue but it can be prevented with timely interventions that are based on evidence. Suicide prevention is also one of the United Nations Sustainable Development Goals (SDG3.4.2) wherein they have asked member countries to work towards reduce global suicide rates by one third by 2030. Notable steps taken by the Government of India include the decriminalization of suicide in the Mental HealthCare Act of 2017 and launching of India's first mental health toll free helpline KIRAN. Many experts have emphasised the urgent need for a national strategy for suicide prevention to be implemented that is multi-sectoral in nature.