A pulmonary alveolus, also known as an air sac or air space, is one of millions of hollow, distensible cup-shaped cavities in the lungs where pulmonary gas exchange takes place. Oxygen is exchanged for carbon dioxide at the blood–air barrier between the alveolar air and the pulmonary capillary. Alveoli make up the functional tissue of the mammalian lungs known as the lung parenchyma, which takes up 90 percent of the total lung volume.

Tuberous sclerosis complex (TSC) is a rare multisystem autosomal dominant genetic disease that causes non-cancerous tumours to grow in the brain and on other vital organs such as the kidneys, heart, liver, eyes, lungs and skin. A combination of symptoms may include seizures, intellectual disability, developmental delay, behavioral problems, skin abnormalities, lung disease, and kidney disease.

Birt–Hogg–Dubé syndrome (BHD), also Hornstein–Birt–Hogg–Dubé syndrome, Hornstein–Knickenberg syndrome, and fibrofolliculomas with trichodiscomas and acrochordons is a human, adult onset, autosomal dominant genetic disorder caused by the FLCN gene. It can cause susceptibility to kidney cancer, renal and pulmonary cysts, and noncancerous tumors of the hair follicles, called fibrofolliculomas. The symptoms seen in each family are unique, and can include any combination of the three symptoms. Fibrofolliculomas are the most common manifestation, found on the face and upper trunk in over 80% of people with BHD over the age of 40. Pulmonary cysts are equally common (84%), but only 24% of people with BHD eventually experience a collapsed lung. Kidney tumors, both cancerous and benign, occur in 14–34% of people with BHD; the associated kidney cancers are often rare hybrid tumors.

Lymphangioleiomyomatosis (LAM) is a rare, progressive and systemic disease that typically results in cystic lung destruction. It predominantly affects women, especially during childbearing years. The term sporadic LAM is used for patients with LAM not associated with tuberous sclerosis complex (TSC), while TSC-LAM refers to LAM that is associated with TSC.

Langerhans cell histiocytosis (LCH) is an abnormal clonal proliferation of Langerhans cells, abnormal cells deriving from bone marrow and capable of migrating from skin to lymph nodes.
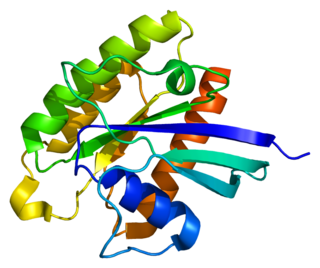
Tuberous sclerosis complex (TSC) tumor suppressors form the TSC1-TSC2 molecular complex. Under poor growth conditions the TSC1-TSC2 complex limits cell growth. A key promoter of cell growth, mTORC1, is inhibited by the tuberous sclerosis complex. Insulin activates mTORC1 and causes dissociation of TSC from the surface of lysosomes.
Inflammatory papillary hyperplasia (IPH) is a benign lesion of the oral mucosa which is characterized by the growth of one or more nodular lesions, measuring about 2mm or less. The lesion almost exclusively involves the hard palate, and in rare instances, it also has been seen on the mandible. The lesion is mostly asymptomatic and color of the mucosa may vary from pink to red.

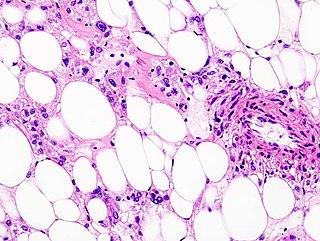
Angiomyolipomas are the most common benign tumour of the kidney. Although regarded as benign, angiomyolipomas may grow such that kidney function is impaired or the blood vessels may dilate and burst, leading to bleeding.

The history of tuberous sclerosis (TSC) research spans less than 200 years. TSC is a rare, multi-system genetic disease that can cause benign tumours to grow on the brain or other vital organs such as the kidneys, heart, eyes, lungs, and skin. A combination of symptoms may include seizures, developmental delay, behavioural problems and skin abnormalities, as well as lung and kidney disease. TSC is caused by mutations on either of two genes, TSC1 and TSC2, which encode for the proteins hamartin and tuberin respectively. These proteins act as tumour growth suppressors and regulate cell proliferation and differentiation. Originally regarded as a rare pathological curiosity, it is now an important focus of research into tumour formation and suppression.

Tuberous sclerosis 1 (TSC1), also known as hamartin, is a protein that in humans is encoded by the TSC1 gene.

A papillary hidradenoma, also termed hidradenoma papilliferum or mammary-like gland adenoma of the vulva, is a rare, but nonetheless most common benign tumor that occurs in and between anal and genital regions of females. These hidradenomas are sharply circumscribed, nodular tumors that usually develop in women's anogenital area but uncommonly occur in other sites in women and men. Papillary hidradenomas that develop outside of the anogenital region are termed ecctopic papillary hidradenomas or ectopic hidradenoma papilliferums.

Adenocarcinoma in situ (AIS) of the lung —previously included in the category of "bronchioloalveolar carcinoma" (BAC)—is a subtype of lung adenocarcinoma. It tends to arise in the distal bronchioles or alveoli and is defined by a non-invasive growth pattern. This small solitary tumor exhibits pure alveolar distribution and lacks any invasion of the surrounding normal lung. If completely removed by surgery, the prognosis is excellent with up to 100% 5-year survival.

Tuberous Sclerosis Complex 2 (TSC2), also known as Tuberin, is a protein that in humans is encoded by the TSC2 gene.
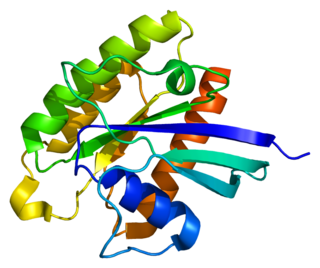
RHEB also known as Ras homolog enriched in brain (RHEB) is a GTP-binding protein that is ubiquitously expressed in humans and other mammals. The protein is largely involved in the mTOR pathway and the regulation of the cell cycle.
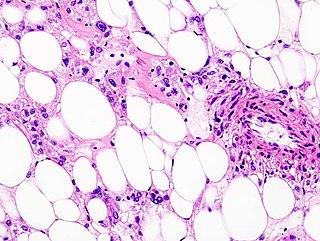
Perivascular epithelioid cell tumour, also known as PEComa or PEC tumour, is a family of mesenchymal tumours consisting of perivascular epithelioid cells (PECs). These are rare tumours that can occur in any part of the human body.

Koenen's tumor (KT), also commonly termed periungual angiofibroma, is a subtype of the angiofibromas. Angiofibromas are benign papule, nodule, and/or tumor lesions that are separated into various subtypes based primarily on the characteristic locations of their lesions. KTs are angiofibromas that develop in and under the toenails and/or fingernails. KTs were once considered as the same as another subtype of the angiofibromas viz., acral angiofibromas. While the literature may still sometimes regard KTs as acral angiofibromas, acral angiofibromas are characteristically located in areas close to but not in the toenails and fingernails as well as in the soles of the feet and palms of the hands. KTs are here regarded as distinct from acral angiofibromas.
Tuberous sclerosis proteins 1 and 2, also known as TSC1 (hamartin) and TSC2 (tuberin), form a protein-complex. The encoding two genes are TSC1 and TSC2. The complex is known as a tumor suppressor. Mutations in these genes can cause tuberous sclerosis complex. Depending on the grade of the disease, intellectual disability, epilepsy and tumors of the skin, retina, heart, kidney and the central nervous system can be symptoms.

Metanephric adenoma (MA) is a rare, benign tumour of the kidney, that can have a microscopic appearance similar to a nephroblastoma, or a papillary renal cell carcinoma.
Atypical adenomatous hyperplasia is a subtype of pneumocytic hyperplasia in the lung. It can be a precursor lesion of in situ adenocarcinoma of the lung. In prostate tissue biopsy, it can be confused for adenocarcinoma of the prostate. The needle biopsy rate is less than 1%.
Pneumocytic hyperplasia is an hyperplasia of pneumocytes lining pulmonary alveoli.