The sarcoplasmic reticulum (SR) is a membrane-bound structure found within muscle cells that is similar to the smooth endoplasmic reticulum in other cells. The main function of the SR is to store calcium ions (Ca2+). Calcium ion levels are kept relatively constant, with the concentration of calcium ions within a cell being 10,000 times smaller than the concentration of calcium ions outside the cell. This means that small increases in calcium ions within the cell are easily detected and can bring about important cellular changes (the calcium is said to be a second messenger; see calcium in biology for more details). Calcium is used to make calcium carbonate (found in chalk) and calcium phosphate, two compounds that the body uses to make teeth and bones. This means that too much calcium within the cells can lead to hardening (calcification) of certain intracellular structures, including the mitochondria, leading to cell death. Therefore, it is vital that calcium ion levels are controlled tightly, and can be released into the cell when necessary and then removed from the cell.
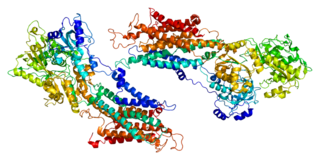
SERCA, or sarco/endoplasmic reticulum Ca2+-ATPase, or SR Ca2+-ATPase, is a calcium ATPase-type P-ATPase. Its major function is to transport calcium from the cytosol into the sarcoplasmic reticulum.

Muscle contraction is the activation of tension-generating sites within muscle cells. In physiology, muscle contraction does not necessarily mean muscle shortening because muscle tension can be produced without changes in muscle length, such as when holding a heavy book or a dumbbell at the same position. The termination of muscle contraction is followed by muscle relaxation, which is a return of the muscle fibers to their low tension-generating state.

Phospholamban, also known as PLN or PLB, is a micropeptide protein that in humans is encoded by the PLN gene. Phospholamban is a 52-amino acid integral membrane protein that regulates the calcium (Ca2+) pump in cardiac muscle cells.
Myocardial contractility represents the innate ability of the heart muscle (cardiac muscle or myocardium) to contract. The ability to produce changes in force during contraction result from incremental degrees of binding between different types of tissue, that is, between filaments of myosin (thick) and actin (thin) tissue. The degree of binding depends upon the concentration of calcium ions in the cell. Within an in vivo intact heart, the action/response of the sympathetic nervous system is driven by precisely timed releases of a catecholamine, which is a process that determines the concentration of calcium ions in the cytosol of cardiac muscle cells. The factors causing an increase in contractility work by causing an increase in intracellular calcium ions (Ca++) during contraction.

Amrinone, also known as inamrinone, and sold as Inocor, is a pyridine phosphodiesterase 3 inhibitor. It is a drug that may improve the prognosis in patients with congestive heart failure. Amrinone has been shown to increase the contractions initiated in the heart by high gain calcium induced calcium release (CICR). The positive inotropic effect of amrinone is mediated by the selective enhancement of high gain CICR which contributes to the contraction of myocytes by phosphorylation through cAMP dependent protein kinase A (PKA) and Ca2+ calmodulin kinase pathways.

Ca2+ ATPase is a form of P-ATPase that transfers calcium after a muscle has contracted. The two kinds of calcium ATPase are:
The Bowditch effect, also known as the Treppe phenomenon and the Treppe effect, is an autoregulation method by which myocardial tension increases with an increase in heart rate. It was first observed by Henry Pickering Bowditch in 1871.
ATP2A2 is an ATPase associated with Darier's disease and Acrokeratosis verruciformis.
Lusitropy is the rate of myocardial relaxation. The increase in cytosolic calcium of cardiomyocytes via increased uptake leads to increased myocardial contractility, but the myocardial relaxation, or lusitropy, decreases. This should not be confused, however, with catecholamine-induced calcium uptake into the sarcoplasmic reticulum, which increases lusitropy.

S100A1, also known as S100 calcium-binding protein A1 is a protein which in humans is encoded by the S100A1 gene. S100A1 is highly expressed in cardiac and skeletal muscle, and localizes to Z-discs and sarcoplasmic reticulum. S100A1 has shown promise as an effective candidate for gene therapy to treat post-myocardially infarcted cardiac tissue.
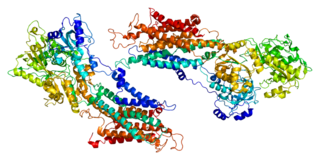
Sarcoplasmic/endoplasmic reticulum calcium ATPase 1 is an enzyme that in humans is encoded by the ATP2A1 gene.

Sarcoplasmic/endoplasmic reticulum calcium ATPase 3 is an enzyme that in humans is encoded by the ATP2A3 gene.

Sarcolipin is a micropeptide protein that in humans is encoded by the SLN gene.

Brody myopathy is a rare disorder that affects skeletal muscle function. BD was first characterized in 1969 by Dr. Irwin A. Brody at Duke University Medical Center. Individuals with BD have difficulty relaxing their muscles after exercise. This difficulty in relaxation leads to symptoms including cramps, stiffness, and discomfort in the muscles of the limbs and face. Symptoms are heightened by exercise and commonly progress in severity throughout adulthood.
JTV-519 (K201) is a 1,4-benzothiazepine derivative that interacts with many cellular targets. It has many structural similarities to diltiazem, a Ca2+ channel blocker used for treatment of hypertension, angina pectoris and some types of arrhythmias. JTV-519 acts in the sarcoplasmic reticulum (SR) of cardiac myocytes by binding to and stabilizing the ryanodine receptor (RyR2) in its closed state. It can be used in the treatment of cardiac arrhythmias, heart failure, catecholaminergic polymorphic ventricular tachycardia (CPVT) and store overload-induced Ca2+ release (SOICR). Currently, this drug has only been tested on animals and its side effects are still unknown. As research continues, some studies have also found a dose-dependent response; where there is no improvement seen in failing hearts at 0.3 μM and a decline in response at 1 μM.
CXL 1020 is an experimental drug that is being investigated as a treatment for acute decompensated heart failure. CXL 1020 functions as a nitroxyl donor; nitroxyl is the reduced, protonated version of nitric oxide. Nitroxyl is capable of enhancing left ventricular contractility without increasing heart rate by modifying normal Ca2+ cycling through the sarcoplasmic reticulum as well as increasing the sensitivity of cardiac myofilaments to Ca2+.

Istaroxime is an investigational drug under development for treatment of acute decompensated heart failure
Calcium buffering describes the processes which help stabilise the concentration of free calcium ions within cells, in a similar manner to how pH buffers maintain a stable concentration of hydrogen ions. The majority of calcium ions within the cell are bound to intracellular proteins, leaving a minority freely dissociated. When calcium is added to or removed from the cytoplasm by transport across the cell membrane or sarcoplasmic reticulum, calcium buffers minimise the effect on changes in cytoplasmic free calcium concentration by binding calcium to or releasing calcium from intracellular proteins. As a result, 99% of the calcium added to the cytosol of a cardiomyocyte during each cardiac cycle becomes bound to calcium buffers, creating a relatively small change in free calcium.
ParvE101Q is an experimental modification of parvalbumin, designed to delay calcium sequestration in heart muscles to enhance contraction. The protein parvalbumin has EF hand motifs used for calcium binding. EF hands are structural helix-loop-helix protein subunits that have a high affinity for calcium ions, and a moderate affinity for magnesium ions. In muscle, the binding of Ca2+ by parvalbumin efficiently sequesters it following contraction. This increases the speed of muscle relaxation, allowing the muscle to contract again sooner. Although parvalbumin is classified as a delayed calcium buffer, it quickly sequesters Ca2+, usually before the muscle is done fully contracting. Large amounts of parvalbumin allow rapid contractions of muscles at a high contractile speed with the trade-off of having relatively lower contraction force. This decreased force of contraction is due to the rapid sequestration of Ca2+, preventing prolonged contraction which is required for greater force.