Related Research Articles
Cambridge University Hospitals NHS Foundation Trust is a British public sector healthcare provider located in Cambridge, England. It was established on 4 November 1992 as Addenbrooke's National Health Service Trust, and authorised as an NHS foundation trust under its current name on 1 July 2004.

The University Hospitals Birmingham NHS Foundation Trust provides adult district general hospital services for Birmingham as well as specialist treatments for the West Midlands.

Primary care trusts (PCTs) were part of the National Health Service in England from 2001 to 2013. PCTs were largely administrative bodies, responsible for commissioning primary, community and secondary health services from providers. Until 31 May 2011, they also provided community health services directly. Collectively PCTs were responsible for spending around 80 per cent of the total NHS budget. Primary care trusts were abolished on 31 March 2013 as part of the Health and Social Care Act 2012, with their work taken over by clinical commissioning groups.

NHS Scotland, sometimes styled NHSScotland, is the publicly–funded healthcare system in Scotland and one of the four systems that make up the National Health Service in the United Kingdom. It operates 14 territorial NHS boards across Scotland, supported by seven special non-geographic health boards, and Public Health Scotland.

The South East Coast Ambulance Service NHS Foundation Trust (SECAmb) is the NHS ambulance services trust for south-eastern England, covering Kent, Surrey, West Sussex and East Sussex. It also covers a part of north-eastern Hampshire around Aldershot, Farnborough, Fleet and Yateley. The service was made an NHS foundation trust on 1 March 2011.
Quasi-markets are markets which can be supervised and organisationally designed that are intended to create greater desire and more efficiency in comparison to conventional delivery systems, while supporting more accessibility, stability and impartiality than traditional markets. Quasi-markets also can be referred to as internal or planned markets.
Nottingham University Hospitals NHS Trust (NUH) is one of England's largest acute teaching trusts. It was established on 1 April 2006 following the merger of Nottingham City Hospital and the Queen's Medical Centre NHS Trusts. They provide acute and specialist services to 2.5m people within Nottingham and surrounding communities at the Queen's Medical Centre (QMC) and the City Hospital campuses, as well as specialist services for a further 3-4m people from across the region.
King's College Hospital NHS Foundation Trust is an NHS trust in London, England. It is closely involved with Guy's and St Thomas' NHS Foundation Trust, with which it shares its chair, Sir Hugh Taylor, its strategy director and IT director. It is assumed that the two organisations will eventually merge.

Healthcare in the United Kingdom is a devolved matter, with England, Northern Ireland, Scotland and Wales each having their own systems of publicly funded healthcare, funded by and accountable to separate governments and parliaments, together with smaller private sector and voluntary provision. As a result of each country having different policies and priorities, a variety of differences have developed between these systems since devolution.
Imperial College Healthcare NHS Trust is an NHS trust based in London, England. It is one of the largest NHS trusts in England and together with Imperial College London forms an academic health science centre.

The National Health Service (NHS) is the publicly funded healthcare system in England, and one of the four National Health Service systems in the United Kingdom. It is the second largest single-payer healthcare system in the world after the Brazilian Sistema Único de Saúde. Primarily funded by the government from general taxation, and overseen by the Department of Health and Social Care, the NHS provides healthcare to all legal English residents and residents from other regions of the UK, with most services free at the point of use for most people. The NHS also conducts research through the National Institute for Health and Care Research (NIHR).
Healthcare in England is mainly provided by the National Health Service (NHS), a public body that provides healthcare to all permanent residents in England, that is free at the point of use. The body is one of four forming the UK National Health Service as health is a devolved matter; there are differences with the provisions for healthcare elsewhere in the United Kingdom, and in England it is overseen by NHS England. Though the public system dominates healthcare provision in England, private health care and a wide variety of alternative and complementary treatments are available for those willing and able to pay.
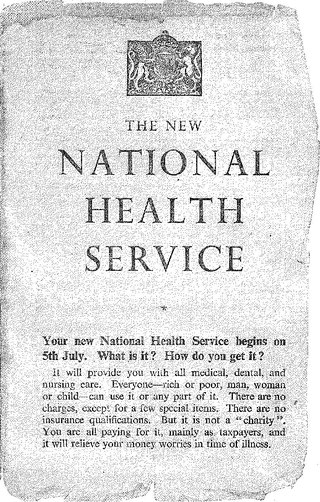
The National Health Service in England was created by the National Health Service Act 1946. Responsibility for the NHS in Wales was passed to the Secretary of State for Wales in 1969, leaving the Secretary of State for Social Services responsible for the NHS in England by itself.
Pennine Acute Hospitals NHS Trust was an acute hospital trust which, until 2019, operated Fairfield General Hospital in Bury, North Manchester General Hospital, the Royal Oldham Hospital and Rochdale Infirmary, all in Greater Manchester. It is now part of the Northern Care Alliance NHS Group. North Manchester General Hospital was formally acquired by Manchester University NHS Foundation Trust on April 1, 2021. The trust also operated Bury General Hospital which closed in 2006.
Health care rationing refers to mechanisms that are used for resource allocation in health care.
The "Greater Manchester Model" of NHS health care was a system uniquely devolved within England, by way of close integration with the Greater Manchester Combined Authority and local authorities, led by the Mayor of Greater Manchester. In July 2022 the Greater Manchester integrated care system took over responsibility for health and social care in the conurbation. The financial plan for 2022–23 had an initial shortage of £187 million.

Private healthcare in the UK, where universal state-funded healthcare is provided by the National Health Service, is a niche market.
Healthcare in Northumberland was the responsibility of the Northumberland, Newcastle Gateshead, and North Tyneside clinical commissioning groups from 2013 to 2022 before being replaced by integrated care systems.
Manchester University NHS Foundation Trust is an NHS Acute Foundation Trust which operates 10 hospitals throughout Greater Manchester. It is the largest NHS trust in the United Kingdom, with an income of £2.2bn and 28,479 staff in 2021–2022.
The private provision of NHS services has been considered a controversial topic since the early 1990s. Keep Our NHS Public, NHS Support Federation and other groups have campaigned against the threat of privatisation, largely in England.
References
- ↑ "Griffiths Report on NHS". Socialist Health Association. Retrieved 2 March 2019.
- ↑ Le Grand, Julian; Bartlett, Will (1993). Quasi-markets and Social Policy. MacMillan. ISBN 0333565193.
- ↑ "London trusts to lose £300m after tariff change". Health Service Journal. 23 January 2019. Retrieved 2 March 2019.
- ↑ "Blair's NHS will adopt the best of the old and the new" . Independent. 30 June 1995. Archived from the original on 18 June 2022. Retrieved 28 February 2019.
- ↑ "Hospital trusts bring internal health market". BBC. 19 May 1998. Retrieved 28 February 2019.
- ↑ "Tony Blair's full speech". Guardian. 28 September 1999. Retrieved 28 February 2019.
- ↑ Klein, Rudolf (27 November 1999). "Markets, politicians, and the NHS". British Medical Journal. 319 (7222): 1383–4. doi:10.1136/bmj.319.7222.1383. PMC 1117121 . PMID 10574834.
- ↑ Arrow, Kenneth (December 1963). "Uncertainty and the welfare economics of medical care" (PDF). The American Economic Review. 53 (5). Retrieved 28 February 2019.
- ↑ McCartney, Margaret (10 July 2017). "An economist explains why healthcare can't be treated as a market". British Medical Journal. Retrieved 28 February 2019.
- ↑ "Cost of the Market in our NHS". Socialist Health Association. 23 February 2015. Retrieved 28 February 2019.
- ↑ "No-one knows the exact cost or benefit of the NHS internal market in England". Full Fact. 27 February 2018. Retrieved 28 February 2019.
- ↑ "Is this the end of the NHS's internal market?". Economist. 2 November 2017. Retrieved 28 February 2019.
- ↑ Triggle, Nick (11 January 2019). "Are Andrew Lansley's NHS reforms being binned?". BBC. Retrieved 11 January 2019.
- ↑ "Scrap laws driving privatisation of health service, say NHS bosses". Guardian. 28 February 2019. Retrieved 28 February 2019.
- ↑ "Dalton steps down and Swindells under threat as Stevens takes over NHSI". Health Service Journal. 1 March 2019. Retrieved 2 March 2019.
- ↑ "Tipping point for the tariff". Health Service Journal. 18 November 2019. Retrieved 8 January 2020.
- ↑ "NHS should 'never return' to tariff system, says top trust CEO". Health Service Journal. 22 July 2020. Retrieved 7 September 2020.
- ↑ Norton, Tom (16 September 2020). "Historic shift from market principles as NHSE sets out new system-level funding". Health Service Journal. Retrieved 26 October 2020.
- ↑ "Government reveals details of plans to scale back NHS competition". Health Service Journal. 22 February 2022. Retrieved 21 April 2022.