Related Research Articles

Varicose veins, also known as varicoses, are a medical condition in which superficial veins become enlarged and twisted. These veins typically develop in the legs, just under the skin. Varicose veins usually cause few symptoms. However, some individuals may experience fatigue or pain in the area. Complications can include bleeding or superficial thrombophlebitis. Varices in the scrotum are known as a varicocele, while those around the anus are known as hemorrhoids. Due to the various physical, social, and psychological effects of varicose veins, they can negatively affect one's quality of life.

Over-the-counter (OTC) drugs are medicines sold directly to a consumer without a requirement for a prescription from a healthcare professional, as opposed to prescription drugs, which may be supplied only to consumers possessing a valid prescription. In many countries, OTC drugs are selected by a regulatory agency to ensure that they contain ingredients that are safe and effective when used without a physician's care. OTC drugs are usually regulated according to their active pharmaceutical ingredient (API) rather than final products. By regulating APIs instead of specific drug formulations, governments allow manufacturers the freedom to formulate ingredients, or combinations of ingredients, into proprietary mixtures.

A prescription, often abbreviated ℞ or Rx, is a formal communication from a physician or other registered healthcare professional to a pharmacist, authorizing them to dispense a specific prescription drug for a specific patient. Historically, it was a physician's instruction to an apothecary listing the materials to be compounded into a treatment—the symbol ℞ comes from the first word of a medieval prescription, Latin recipere, that gave the list of the materials to be compounded.
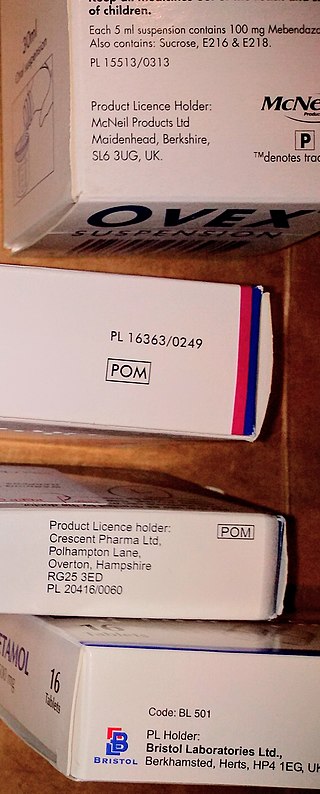
A prescription drug is a pharmaceutical drug that is permitted to be dispensed only to those with a medical prescription. In contrast, over-the-counter drugs can be obtained without a prescription. The reason for this difference in substance control is the potential scope of misuse, from drug abuse to practicing medicine without a license and without sufficient education. Different jurisdictions have different definitions of what constitutes a prescription drug.
The British Homeopathic Association (BHA) is a British charity founded in 1902 by John Epps to promote homeopathy and advocate for its training and research. The BHA was re-branded in 2021 to Homeopathy UK. It supports the use of homeopathy within general and specialist healthcare, and provides a listing of homeopathic practitioners. From 1902, the BHA co-sponsored the Missionary School of Medicine, a school of medicine for medical missionaries. The charity also campaigns for more homeopathy in Britain's National Health Service (NHS).
The NHS Electronic Prescription Service is part of the NHS National Programme for IT of the National Health Service in England. It enables the electronic transfer of medical prescriptions from doctors to pharmacies and other dispensers and electronic notification to the reimbursement agency, NHS Prescription Services.
Charges for prescriptions for medicines and some medical appliances are payable by adults in England under the age of 60. However, people may be exempt from charges in various exemption categories. Charges were abolished by NHS Wales in 2007, Health and Social Care in Northern Ireland in 2010 and by NHS Scotland in 2011. In 2010/11, in England, £450 million was raised through these charges, some 0.5% of the total NHS budget. In April 2021 the charge was raised to £9.35 for up to a three-month supply of each item. In 2022, for the first time since 2010, the charge was not increased.

Healthcare in the United Kingdom is a devolved matter, with England, Northern Ireland, Scotland and Wales each having their own systems of publicly funded healthcare, funded by and accountable to separate governments and parliaments, together with smaller private sector and voluntary provision. As a result of each country having different policies and priorities, a variety of differences have developed between these systems since devolution.

The National Health Service (NHS) is the publicly funded healthcare system in England, and one of the four National Health Service systems in the United Kingdom. It is the second largest single-payer healthcare system in the world after the Brazilian Sistema Único de Saúde. Primarily funded by the government from general taxation, and overseen by the Department of Health and Social Care, the NHS provides healthcare to all legal English residents and residents from other regions of the UK, with most services free at the point of use for most people. The NHS also conducts research through the National Institute for Health and Care Research (NIHR).
Healthcare in England is mainly provided by the National Health Service (NHS), a public body that provides healthcare to all permanent residents in England, that is free at the point of use. The body is one of four forming the UK National Health Service as health is a devolved matter; there are differences with the provisions for healthcare elsewhere in the United Kingdom, and in England it is overseen by NHS England. Though the public system dominates healthcare provision in England, private health care and a wide variety of alternative and complementary treatments are available for those willing and able to pay.

Homeopathy is fairly common in some countries while being uncommon in others. In some countries, there are no specific legal regulations concerning the use of homeopathy, while in others, licenses or degrees in conventional medicine from accredited universities are required.
A formulary is a list of pharmaceutical drugs, often decided upon by a group of people, for various reasons such as insurance coverage or use at a medical facility. Traditionally, a formulary contained a collection of formulas for the compounding and testing of medication. Today, the main function of a prescription formulary is to specify particular medications that are approved to be prescribed at a particular hospital, in a particular health system, or under a particular health insurance policy. The development of prescription formularies is based on evaluations of efficacy, safety, and cost-effectiveness of drugs.
Electronic prescription is the computer-based electronic generation, transmission, and filling of a medical prescription, taking the place of paper and faxed prescriptions. E-prescribing allows a physician, physician assistant, pharmacist, or nurse practitioner to use digital prescription software to electronically transmit a new prescription or renewal authorization to a community or mail-order pharmacy. It outlines the ability to send error-free, accurate, and understandable prescriptions electronically from the healthcare provider to the pharmacy. E-prescribing is meant to reduce the risks associated with traditional prescription script writing. It is also one of the major reasons for the push for electronic medical records. By sharing medical prescription information, e-prescribing seeks to connect the patient's team of healthcare providers to facilitate knowledgeable decision making.
Health care rationing refers to mechanisms that are used for resource allocation in health care.

Michael Dixon LVO, OBE, FRCGP, FRCP is an English general practitioner and current Head of the Royal Medical Household. He is Chair of The College of Medicine and Integrated Health and Visiting Professor at the University of Westminster.
There are approximately 88,000 pharmacies in the United States. Over half are located within drug stores, grocery stores, hospitals, department stores, medical clinics, surgery clinics, universities, nursing homes, prisons, and other facilities. The remaining pharmacies are considered to be independent or privately owned. The top 25 pharmacy chain stores represent about 38,000 pharmacy locations in the U.S. and employ about 149,000 on-staff pharmacists. California has 8,015 pharmacies, the most of any state. Texas, Florida, New York, and Pennsylvania round out the top five states for pharmacy locations. Nationwide, the number of community pharmacies increased by 6.3% between 2007-2015, and the number of pharmacies per 10,000 people (2.11) did not change. However, the number of pharmacies per-capita varies substantially across counties, ranging from 0 to 13.6 per- 10,000 people in 2015.
Pharmacy2U is an online pharmacy located in the UK. Pharmacy2U has been involved in piloting the electronic transfer of prescriptions in the UK. They manage NHS repeat prescriptions on behalf of patients. Pharmacy2U was founded by pharmacist Daniel Lee in November 1999. It launched to the public in June 2000.

The Good Thinking Society is a nonprofit organisation promoting scientific scepticism established by Simon Singh in September 2012.
Pharmacy in the United Kingdom has been an integral part of the National Health Service since it was established in 1948. Unlike the rest of the NHS, pharmacies are largely privately provided apart from those in hospitals, and even these are now often privately run.

A Minor Ailment Scheme is a service provided by pharmacies for the National Health Service, first established in England in 2008.
References
- ↑ "How the NHS places a value on life". BBC News. 21 August 2006. Retrieved 28 August 2017.
- ↑ "NHS Scotland to offer three cycles of IVF". Bionews. 27 March 2017. Retrieved 28 August 2017.
- ↑ "Varicose veins: Could a new 'superglue' end the pain?". Daily Mirror. 27 June 2013. Retrieved 28 August 2017.
- ↑ "CCGs restricting access to basic treatments". Health Service Journal. 20 March 2019. Retrieved 6 May 2019.
- ↑ "NHS operation fury as price list revealed - with patients charged up to £8,000". Birmingham Live. 19 June 2019. Retrieved 19 June 2019.
- ↑ "Exclusive: Trusts charging for ops restricted on the NHS". Health Service Journal. 8 July 2019. Retrieved 10 July 2019.
- ↑ "National Health Service (General Medical Services Contracts) (Prescription of Drugs etc.) Regulations 2004". Legislation.gov.uk. Retrieved 12 April 2019.
- ↑ A, A. Applied Pharmaceutical Practice.
- ↑ "Medicinal products". Pharmaceutical Services Negotiating Committee. Retrieved 25 August 2017.
- ↑ James Gallagher (13 November 2015). "Homeopathy 'could be blacklisted'". BBC News.
- ↑ Damien Gayle (14 November 2015). "Homeopathy on prescription could be banned from NHS". The Guardian.
- ↑ "GPs could be banned from giving out homeopathy on prescription". Daily Telegraph. 13 November 2015.
- ↑ "NHS still spending £55,000 a year on homeopathy, despite ban". Telegraph. 5 April 2019. Retrieved 17 May 2019.
- ↑ "NHS England names 'ineffective' medicines for savings drive". Health Service Journal. 21 July 2017. Retrieved 28 August 2017.
- ↑ "DH 'blacklist' required to enable GPs to curb OTC prescribing, says GPC lead". Pulse. 21 April 2017. Retrieved 29 April 2017.
- ↑ "NHS ban on 'wasteful' prescribing could harm poorest patients, GPs warn". GP Online. 21 July 2017. Retrieved 25 August 2017.
- ↑ "NHS England issues guidance to curb over-the-counter prescribing". Pulse. 29 March 2018. Retrieved 31 March 2018.
- ↑ "OTC medication rationing only made a quarter of its targeted savings". Pulse. 17 April 2019. Retrieved 4 June 2019.
- ↑ "Restrictions on prescribing OTC treatments rejected in Wales". Pharmaceutical Journal. 24 April 2019. Retrieved 9 June 2019.