Antipsychotics, also known as neuroleptics, are a class of psychotropic medication primarily used to manage psychosis, principally in schizophrenia but also in a range of other psychotic disorders. They are also the mainstay together with mood stabilizers in the treatment of bipolar disorder.

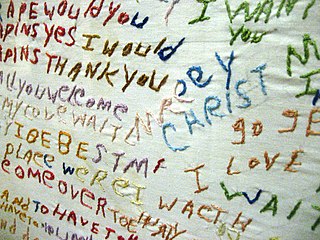
Psychosis is an abnormal condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior that is inappropriate for a given situation. There may also be sleep problems, social withdrawal, lack of motivation, and difficulties carrying out daily activities. Psychosis can have serious adverse outcomes.
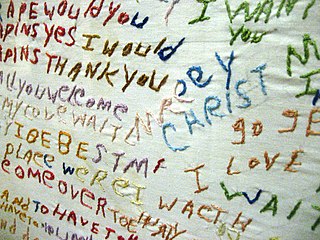
Schizophrenia is a mental disorder characterized by continuous or relapsing episodes of psychosis. Major symptoms include hallucinations, delusions, paranoia, and disorganized thinking. Other symptoms include social withdrawal, decreased emotional expression, and apathy. Symptoms typically come on gradually, begin in young adulthood, and in many cases never resolve. There is no objective diagnostic test; the diagnosis is used to describe observed behavior that may stem from numerous different causes. Besides observed behavior, doctors will also take a history that includes the person's reported experiences, and reports of others familiar with the person, when making a diagnosis. To diagnose someone with schizophrenia, doctors are supposed to confirm that symptoms and functional impairment are present for six months (DSM-5) or one month (ICD-11). Many people with schizophrenia have other mental disorders, especially substance use disorders, depressive disorders, anxiety disorders, and obsessive–compulsive disorder.

Clozapine is a psychiatric medication and is the first atypical antipsychotic. It is primarily used to treat people with schizophrenia and schizoaffective disorders who have had an inadequate response to other antipsychotics or who have been unable to tolerate other drugs due to extrapyramidal side effects. It is also used for the treatment of psychosis in Parkinson's disease. Clozapine is regarded as the gold-standard treatment when other medication has been insufficiently effective and its use is recommended by multiple international treatment guidelines, after resistance to earlier neuroleptic treatment is established.
Schizoaffective disorder is a mental disorder characterized by abnormal thought processes and an unstable mood. This diagnosis is made when the person has symptoms of both schizophrenia and a mood disorder: either bipolar disorder or depression. The main criterion for a diagnosis of schizoaffective disorder is the presence of psychotic symptoms for at least two weeks without any mood symptoms present. Schizoaffective disorder can often be misdiagnosed when the correct diagnosis may be psychotic depression, bipolar I disorder, schizophreniform disorder, or schizophrenia. It is imperative for providers to accurately diagnose patients, as treatment and prognosis differ greatly for each of these diagnoses.

The Institute of Psychiatry, Psychology and Neuroscience (IoPPN) is a research institution dedicated to discovering what causes mental illness and diseases of the brain. In addition, its aim is to help identify new treatments for them and ways to prevent them in the first place. The IoPPN is a faculty of King's College London, England, previously known as the Institute of Psychiatry (IoP).

The Maudsley Hospital is a British psychiatric hospital in south London. The Maudsley is the largest mental health training institution in the UK. It is part of South London and Maudsley NHS Foundation Trust, and works in partnership with the Institute of Psychiatry, King's College London. The hospital was one of the originating institutions in producing the Maudsley Prescribing Guidelines. It is part of the King's Health Partners academic health science centre and the National Institute for Health Research (NIHR) Biomedical Research Centre for Mental Health.
Professor Christos Pantelis is an Australian professor of medicine who is the Director of the Melbourne Neuropsychiatry Centre.

Sir Robin MacGregor Murray FRS is a Scottish psychiatrist, Professor of Psychiatric Research at the Institute of Psychiatry, King's College London. He has treated patients with schizophrenia and bipolar illness referred to the National Psychosis Unit of the South London and Maudsley NHS Trust because they fail to respond to treatment, or cannot get appropriate treatment, locally; he sees patients privately if they are unable to obtain an NHS referral.
Eliot Trevor Oakeshott Slater MD was a British psychiatrist who was a pioneer in the field of the genetics of mental disorders. He held senior posts at the National Hospital for Nervous Diseases, Queen Square, London, and the Institute of Psychiatry at the Maudsley Hospital. He was the author of some 150 scientific papers and the co-author of several books on psychiatric topics, notably on disputed 'physical methods'. From the mid-50s to his death, he co-edited Clinical Psychiatry, the leading textbook for psychiatric trainees.

South London and Maudsley NHS Foundation Trust, is an NHS foundation trust based in London, England, which specialises in mental health. It comprises three psychiatric hospitals, the Ladywell Unit based at University Hospital Lewisham, and serves the boroughs of Lambeth, Lewisham, Croydon and Southwark. The Trust also provides drug and alcohol services and 50 high-quality, national specialist services for people with complex needs.

Michael Shepherd, CBE, FRCP, FRCPsych (Hon), FAPA (Corr), FAPHA was one of the most influential and internationally respected psychiatrists of his time, formerly Professor of Epidemiological Psychiatry, Institute of Psychiatry and Consultant Psychiatrist, The Maudsley Hospital, London and author of a number of influential publications in the field of psychiatry, including the seminal work Psychiatric Illness in General Practice.
Pamela Jane Taylor, is a British psychiatrist and academic, who specialises in the links between psychosis and violence, and mental and physical health in the criminal justice system. Since 2004, she has been Professor of Forensic Psychiatry in the Department Institute of Psychological Medicine and Clinical Neurosciences of Cardiff University.
Allen J. Frances is an American psychiatrist. He is currently Professor and Chairman Emeritus of the Department of Psychiatry and Behavioral Sciences at Duke University School of Medicine. He is best known for serving as chair of the American Psychiatric Association task force overseeing the development and revision of the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). Frances is the founding editor of two well-known psychiatric journals: the Journal of Personality Disorders and the Journal of Psychiatric Practice.

Lambeth Hospital is a mental health facility in Landor Road, South London. It was previously known as the "Landor Road hospital" and is now operated by the South London and Maudsley NHS Foundation Trust and is affiliated with King's College London's Institute of Psychiatry. It is also part of the King's Health Partners academic health science centre and the National Institute for Health Research (NIHR) Biomedical Research Centre for Mental Health.
Celso Arango is a psychiatrist who has worked as a clinician, researcher, and educator in psychiatry and mental health, notably in the field of child and adolescent psychiatry, psychosis, and mental health promotion.

Ulrike Schmidt MRCPsych Dr. Med. Ph.D is a psychiatrist at the Institute of Psychiatry, Psychology and Neuroscience, King's College London in London, where she is Professor of Eating Disorders as well as the Head of the Section of Eating Disorders. Schmidt is a consultant at the Eating Disorders Service within the South London and Maudsley NHS Foundation Trust. Schmidt is known for her ground breaking work helping people with eating disorders and their clinicians.
Anne Farmer is emeritus professor of psychiatric nosology at the Institute of Psychiatry and was formerly lead consultant in the Affective Disorders Unit at the South London and Maudsley NHS Foundation Trust and the trust's director of medical education. Farmer's focus is on genetic research in affective disorders. Farmer was previously professor of psychiatry at the University of Wales College of Medicine.

Kate Tchanturia is a Professor of Psychology in Eating Disorders at the Institute of Psychiatry, Psychology and Neuroscience, King’s College London. She is also Consultant Psychologist at the South London and Maudsley NHS Foundation Trust for the National Eating Disorder Service London, United Kingdom. Her main research interests include cultural differences in illness presentations, cognitive profiles in eating disorders, and experimental work in emotion processing and translational research from experimental findings to real clinical practice. Tchanturia has a particular interest in women’s mental health and has pioneered the novel pathway for the autism spectrum condition (ASC) and eating disorder comorbidity.

David Taylor FFRPS FRPharmS is a British professor. He is the head of the Pharmaceutical Sciences Clinical Academic Group within King's Health Partners. Taylor has been lead author and editor of the Maudsley Prescribing Guidelines in Psychiatry since 1994. In 2014, Taylor was named as one of the top 100 clinical leaders in the UK National Health Service.