Research
Carpal tunnel syndrome
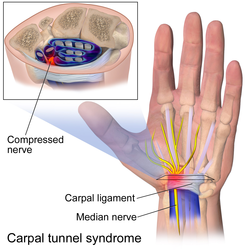
Carpal tunnel syndrome (CTS) is a condition that induces pain when the median nerve passes through the carpal tunnel in the wrist. It occurs when median nerves get irritated, compress, and strengthen. CTS evokes symptoms, including pain, paresthesia, and muscle atrophy. [1] This further leads to chronic pain and economic difficulties for patients as it requires work absence and surgical treatment.[ citation needed ]
Nerve gliding exercise becomes one of the optimal CTS treatments by assisting nerve mobilization. Restoring nerve mobilization would relieve edema and restore adhesion in the carpal tunnel. [2] According to the research, nerve gliding exercise has reduced the pain, decreased sensitive distal latency, and improved the functions that require force to grab. However, inappropriate nerve gliding exercises would worsen the conditions. Neural mobilization via nerve gliding should avoid excessive median nerve stretching when extending fingers in wrist extensions or when otherwise not advised. [3]
Nerve gliding exercise is not an optimal method for every patient. There is limited evidence on the effectiveness of neural gliding. However, the addition of nerve gliding exercise in conservative care accelerates the rehabilitation process and avoids surgical treatment. Further research is required to study the effectiveness of nerve glide physiotherapy and to determine groups that tend to respond better. [4]

Acute sciatica and hip range of motion
Sciatica is low back pain that can extend to the feet. [5] This nerve pain is caused by nerve root irritation or constriction. Sciatica is known as an extremely painful symptom. Nerve glides are a common option for sciatica due to their cost-effectiveness. After performing nerve glides, the Numeric Pain Rating Score (NPRS) rated by patients improved, indicating a reduction in the pain. The nerve glide reduces acute sciatica and improves the range of motion of the hip. When nerve glides were performed along with other therapies, it resulted in a greater reduction in pain. [6] However, the research indicates that there is no statistically significant difference in the results among patients who were treated with nerve glides and other conventional treatments. [7]
Neck and arm pain
Neural gliding is used for the rehabilitation of nerve-related neck and arm pain. The pain initiates from the neck, expanding to the arm. Nerve gliding physical therapy is beneficial in reducing pain intensity, bringing short-term improvements. [8] This treatment was found to manage neural tissue through specific postures and movements of the parts in pain. The stretch reduces nerve mechanosensitive that relieves discomforts, eventually leading to the normal function of the body. However, the long-term effects of nerve gliding exercises still remain unclear. [9]
Cubital tunnel syndrome

Cubital tunnel syndrome is a condition that can cause pain when the ulnar nerves are stretched, pressed, or irritated. This syndrome is also known as "ulnar nerve entrapment". Similar to carpal tunnel syndrome, cubital tunnel syndrome can cause pain, numbness, tingling, or weakness in the hand. [10] Patients with cubital tunnel syndrome may experience loss of grip strength and weakness in the affected hand. The ulnar nerve passes through the cubital tunnel in the elbow. Irritation or injuries at the elbow can lead to cubital tunnel syndrome. [11]
Ulnar nerve gliding is recommended to reduce symptoms of cubital tunnel syndrome. Patients with ulnar nerve gliding should stay away from the holding position. Rather, patients must repeat nerve gliding with the range of movement. There are various ulnar nerve gliding methods, which include elbow flexion, wrist extension, head tilt, and arm flexion.[ citation needed ]