Effectiveness
A 2015 study helped to characterize the impact of nocturnist. Compared with before implementation, there was no difference in mortality, 30-day readmissions, mean length of stay, or upgrades to intensive care with the addition of these overnight hospitalists. [5] Similar results were reproduced in a 2018-19 Canadian study, that nocturnists being present did not affect patient outcomes.
In a 2020 survey of 20,744 internal medicine residents, it was found that more residents reported receiving adequate supervision when nocturnists were present, although the reported percentage was rather low, with the authors speculating this is due to the variable implementations of nocturnist occupations. [6]
Salary
According to a 2011 survey, the average salary for a nocturnist was 2.5% lower than other hospitalists, and the survey results report nocturnists were 27% less productive than other day-time physician roles as measured by work relative value units. [7]
Related Research Articles
Evidence-based medicine (EBM) is "the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients." The aim of EBM is to integrate the experience of the clinician, the values of the patient, and the best available scientific information to guide decision-making about clinical management. The term was originally used to describe an approach to teaching the practice of medicine and improving decisions by individual physicians about individual patients.
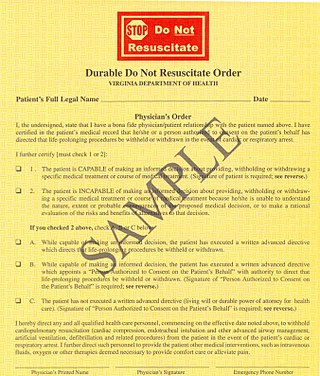
A do-not-resuscitate order (DNR), also known as Do Not Attempt Resuscitation (DNAR), Do Not Attempt Cardiopulmonary Resuscitation (DNACPR), no code or allow natural death, is a medical order, written or oral depending on the jurisdiction, indicating that a person should not receive cardiopulmonary resuscitation (CPR) if that person's heart stops beating. Sometimes these decisions and the relevant documents also encompass decisions around other critical or life-prolonging medical interventions. The legal status and processes surrounding DNR orders vary in different polities. Most commonly, the order is placed by a physician based on a combination of medical judgement and patient involvement.
Internal medicine, also known as general internal medicine in Commonwealth nations, is a medical specialty for medical doctors focused on the prevention, diagnosis, and treatment of internal diseases in adults. Medical practitioners of internal medicine are referred to as internists, or physicians in Commonwealth nations. Internists possess specialized skills in managing patients with undifferentiated or multi-system disease processes. They provide care to both hospitalized (inpatient) and ambulatory (outpatient) patients and often contribute significantly to teaching and research. Internists are qualified physicians who have undergone postgraduate training in internal medicine, and should not be confused with "interns”, a term commonly used for a medical doctor who has obtained a medical degree but does not yet have a license to practice medicine unsupervised.

Ambulatory care or outpatient care is medical care provided on an outpatient basis, including diagnosis, observation, consultation, treatment, intervention, and rehabilitation services. This care can include advanced medical technology and procedures even when provided outside of hospitals.
A medical error is a preventable adverse effect of care ("iatrogenesis"), whether or not it is evident or harmful to the patient. This might include an inaccurate or incomplete diagnosis or treatment of a disease, injury, syndrome, behavior, infection, or other ailment.
Hospital medicine is a medical specialty that exists in some countries as a branch of family medicine or internal medicine, dealing with the care of acutely ill hospitalized patients. Physicians whose primary professional focus is caring for hospitalized patients only while they are in the hospital are called hospitalists. Originating in the United States, this type of medical practice has extended into Australia and Canada. The vast majority of physicians who refer to themselves as hospitalists focus their practice upon hospitalized patients. Hospitalists are not necessarily required to have separate board certification in hospital medicine.

A primary care physician (PCP) is a physician who provides both the first contact for a person with an undiagnosed health concern as well as continuing care of varied medical conditions, not limited by cause, organ system, or diagnosis. The term is primarily used in the United States. In the past, the equivalent term was 'general practitioner' in the US; however in the United Kingdom and other countries the term general practitioner is still used. With the advent of nurses as PCPs, the term PCP has also been expanded to denote primary care providers.
Medical resident work hours refers to the shifts worked by medical interns and residents during their medical residency.
Patient safety is a discipline that emphasizes safety in health care through the prevention, reduction, reporting and analysis of error and other types of unnecessary harm that often lead to adverse patient events. The frequency and magnitude of avoidable adverse events, often known as patient safety incidents, experienced by patients was not well known until the 1990s, when multiple countries reported significant numbers of patients harmed and killed by medical errors. Recognizing that healthcare errors impact 1 in every 10 patients around the world, the World Health Organization (WHO) calls patient safety an endemic concern. Indeed, patient safety has emerged as a distinct healthcare discipline supported by an immature yet developing scientific framework. There is a significant transdisciplinary body of theoretical and research literature that informs the science of patient safety with mobile health apps being a growing area of research.
A clinical prediction rule or clinical probability assessment specifies how to use medical signs, symptoms, and other findings to estimate the probability of a specific disease or clinical outcome.
The Zambia Electronic Perinatal Record System (ZEPRS) is an Electronic Medical Record (EMR) system used by public obstetric clinics and a hospital in Lusaka, Zambia.
The July effect, sometimes referred to as the July phenomenon, is a perceived but scientifically unfounded increase in the risk of medical errors and surgical complications that occurs in association with the time of year in which United States medical school graduates begin residencies. A similar period in the United Kingdom is known as the killing season or, more specifically, Black Wednesday, referring to the first Wednesday in August when postgraduate trainees commence their rotations.

Choosing Wisely is a United States-based health educational campaign, led by the ABIM Foundation, about unnecessary health care.
Health care quality is a level of value provided by any health care resource, as determined by some measurement. As with quality in other fields, it is an assessment of whether something is good enough and whether it is suitable for its purpose. The goal of health care is to provide medical resources of high quality to all who need them; that is, to ensure good quality of life, cure illnesses when possible, to extend life expectancy, and so on. Researchers use a variety of quality measures to attempt to determine health care quality, including counts of a therapy's reduction or lessening of diseases identified by medical diagnosis, a decrease in the number of risk factors which people have following preventive care, or a survey of health indicators in a population who are accessing certain kinds of care.
An obstetric hospitalist is an obstetrician and gynaecologist physician who is either employed by a hospital or a physician practice and whose duties include providing care for laboring patients and managing obstetric emergencies. Some obstetrics hospitalists also have responsibilities including resident and medical student teaching; providing backup support for family practitioners and nurse midwives, assisting private physicians with surgery, assuming care for ob-gyn patients unassigned to a physician and providing vacation coverage for the private practicing physician.
Physician burnout has been classified as a psychological syndrome that can be expressed as a prolonged response to due chronic occupational stressors. In the practice of medicine, it has been known to affect a wide variety of individuals from medical students to practicing physicians; although, its impact reaches far beyond that. Because of the toll taken on the healthcare industry, various treatment and prevention strategies have been developed at individual, team, and organizational levels in hopes to seek the best method of addressing this epidemic.

Vineet M. Arora is an American medical researcher who is the Herbert T. Abelson Professor of Medicine and Dean for Medical Education at the University of Chicago Pritzker School of Medicine. She is a Fellow of the National Academy of Medicine. Her research considers clinical medicine and medical education, with a focus on the improvement of the quality of care in teaching hospitals.

A teaching hospital is a hospital or medical centre that provides medical education and training to future and current health professionals. Teaching hospitals are almost always affiliated with one or more universities and are often co-located with medical schools.
Kevin G. Volpp is an American behavioral economist and Mark V. Pauly President's Distinguished Professor at the University of Pennsylvania’s Perelman School of Medicine and the Wharton School. He is the Director of the Penn Center for Health Incentives & Behavioral Economics (CHIBE)..
In the domain of hospital medicine, interdisciplinary bedside rounds are a collaborative approach to patient care that involves the participation of the bedside nurse, primary provider, and the patient. They are often joined by family members and allied health professionals such as the patient's pharmacist and case manager.
References
- 1 2 Dunbar-Yaffe, Richard; Wu, Robert C.; Oza, Amit; Lee-Kim, Victoria; Cram, Peter (April 2021). "Impact of an internal medicine nocturnist service on care of patients with cancer at a large Canadian teaching hospital: a quality-improvement study". CMAJ Open. 9 (2): E667–E672. doi: 10.9778/cmajo.20200167 . ISSN 2291-0026.
- ↑ Sabharwal, Aman (June 2005). "Life as a Nocturnist" (PDF). The Hospitalist. 9 (3): 43–44.
- ↑ Walkinshaw, Erin (September 20, 2011). "Middle-of-the-night medicine is rarely patient-centred". CMAJ. 183 (13): 1467–1468. doi:10.1503/cmaj.109-3953. PMC 3176838 . PMID 21859867 . Retrieved 19 September 2021.
- ↑ Beresford, Larry (8 January 2019). "The state of hospital medicine in 2018". The Hospitalist. Society of Hospital Medicine. Retrieved 22 June 2020.
- ↑ Gonzalo, Jed (20 May 2015). "Impact of an Overnight Internal Medicine Academic Hospitalist Program on Patient Outcomes". J Gen Intern Med. 30 (12): 1795–1802. doi: 10.1007/s11606-015-3389-0 . PMC 4636563 . PMID 25990190.
- ↑ Catalanotti, Jillian S.; O’Connor, Alec B.; Kisielewski, Michael; Chick, Davoren A.; Fletcher, Kathlyn E. (2020-04-14). "Association Between Nocturnist Supervision and Perceived Overnight Supervision Adequacy Among Internal Medicine Residents in the US". JAMA. 323 (14): 1407. doi: 10.1001/jama.2020.0875 . ISSN 0098-7484.
- ↑ Flores, Leslie (2 September 2011). "Nocturnists' Compensation Puzzles Practice Leaders". The Hospitalist. Society of Hospital Medicine. Retrieved June 19, 2020.