Telehealth is the distribution of health-related services and information via electronic information and telecommunication technologies. It allows long-distance patient and clinician contact, care, advice, reminders, education, intervention, monitoring, and remote admissions. Telemedicine is sometimes used as a synonym, or is used in a more limited sense to describe remote clinical services, such as diagnosis and monitoring. When rural settings, lack of transport, a lack of mobility, conditions due to outbreaks, epidemics or pandemics, decreased funding, or a lack of staff restrict access to care, telehealth may bridge the gap as well as provide distance-learning; meetings, supervision, and presentations between practitioners; online information and health data management and healthcare system integration. Telehealth could include two clinicians discussing a case over video conference; a robotic surgery occurring through remote access; physical therapy done via digital monitoring instruments, live feed and application combinations; tests being forwarded between facilities for interpretation by a higher specialist; home monitoring through continuous sending of patient health data; client to practitioner online conference; or even videophone interpretation during a consult.

A medical guideline is a document with the aim of guiding decisions and criteria regarding diagnosis, management, and treatment in specific areas of healthcare. Such documents have been in use for thousands of years during the entire history of medicine. However, in contrast to previous approaches, which were often based on tradition or authority, modern medical guidelines are based on an examination of current evidence within the paradigm of evidence-based medicine. They usually include summarized consensus statements on best practice in healthcare. A healthcare provider is obliged to know the medical guidelines of their profession, and has to decide whether to follow the recommendations of a guideline for an individual treatment.
eHealth describes healthcare services which are supported by digital processes, communication or technology such as electronic prescribing, Telehealth, or Electronic Health Records (EHRs). The use of electronic processes in healthcare dated back to at least the 1990s. Usage of the term varies as it covers not just "Internet medicine" as it was conceived during that time, but also "virtually everything related to computers and medicine". A study in 2005 found 51 unique definitions. Some argue that it is interchangeable with health informatics with a broad definition covering electronic/digital processes in health while others use it in the narrower sense of healthcare practice using the Internet. It can also include health applications and links on mobile phones, referred to as mHealth or m-Health. Key components of eHealth include electronic health records (EHRs), telemedicine, health information exchange, mobile health applications, wearable devices, and online health information. These technologies enable healthcare providers, patients, and other stakeholders to access, manage, and exchange health information more effectively, leading to improved communication, decision-making, and overall healthcare outcomes.

Telenursing refers to the use of information technology in the provision of nursing services whenever physical distance exists between patient and nurse, or between any number of nurses. As a field, it is part of telemedicine, and has many points of contacts with other medical and non-medical applications, such as telediagnosis, teleconsultation, and telemonitoring. The field, however, is still being developed as the information on telenursing isn't comprehensive enough.
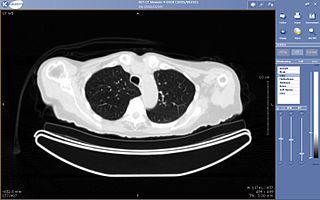
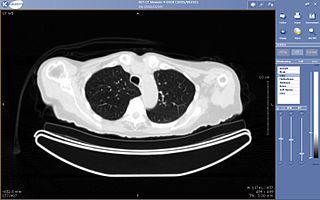
Teleradiology is the transmission of radiological patient images from procedures such as x-rays photographs, Computed tomography (CT), and MRI imaging, from one location to another for the purposes of sharing studies with other radiologists and physicians. Teleradiology allows radiologists to provide services without actually having to be at the location of the patient. This is particularly important when a sub-specialist such as an MRI radiologist, neuroradiologist, pediatric radiologist, or musculoskeletal radiologist is needed, since these professionals are generally only located in large metropolitan areas working during daytime hours. Teleradiology allows for specialists to be available at all times.

The Royal Australian College of General Practitioners (RACGP) is the professional body for general practitioners (GPs) in Australia. The RACGP is responsible for maintaining standards for quality clinical practice, education and training, and research in Australian general practice. The RACGP represents over 40,000 members across metropolitan, urban, rural and remote Australia.
The American Telemedicine Association (ATA), established in 1993, is a non-profit organization whose goal is to promote access to medical care for consumers and health professionals via telecommunications technology. Membership in the American Telemedicine Association is open to individuals, companies, and other healthcare and technology organizations.
A Patient Safety Organization (PSO) is a group, institution, or association that improves medical care by reducing medical errors. Common functions of patient safety organizations are data collection, analysis, reporting, education, funding, and advocacy. A PSO differs from a Federally designed Patient Safety Organization (PSO), which provides health care providers in the U.S. privilege and confidentiality protections for efforts to improve patient safety and the quality of patient care delivery

Telepsychiatry or telemental health refers to the use of telecommunications technology to deliver psychiatric care remotely for people with mental health conditions. It is a branch of telemedicine.

In medicine, rural health or rural medicine is the interdisciplinary study of health and health care delivery in rural environments. The concept of rural health incorporates many fields, including wilderness medicine, geography, midwifery, nursing, sociology, economics, and telehealth or telemedicine.
The healthcare reform in China refers to the previous and ongoing healthcare system transition in modern China. China's government, specifically the National Health and Family Planning Commission, plays a leading role in these reforms. Reforms focus on establishing public medical insurance systems and enhancing public healthcare providers, the main component in China's healthcare system. In urban and rural areas, three government medical insurance systems—Urban Residents Basic Medical Insurance, Urban Employee Basic Medical Insurance, and the New Rural Co-operative Medical Scheme—cover almost everyone. Various public healthcare facilities, including county or city hospitals, community health centers, and township health centers, were founded to serve diverse needs. Current and future reforms are outlined in Healthy China 2030.

mHealth is an abbreviation for mobile health, a term used for the practice of medicine and public health supported by mobile devices. The term is most commonly used in reference to using mobile communication devices, such as mobile phones, tablet computers and personal digital assistants (PDAs), and wearable devices such as smart watches, for health services, information, and data collection. The mHealth field has emerged as a sub-segment of eHealth, the use of information and communication technology (ICT), such as computers, mobile phones, communications satellite, patient monitors, etc., for health services and information. mHealth applications include the use of mobile devices in collecting community and clinical health data, delivery/sharing of healthcare information for practitioners, researchers and patients, real-time monitoring of patient vital signs, the direct provision of care as well as training and collaboration of health workers.
Health informatics in China is about the Health informatics or Medical informatics or Healthcare information system/technology in China.
Connected health is a socio-technical model for healthcare management and delivery by using technology to provide healthcare services remotely. Connected health, also known as technology enabled care (TEC) aims to maximize healthcare resources and provide increased, flexible opportunities for consumers to engage with clinicians and better self-manage their care. It uses readily available consumer technologies to deliver patient care outside of the hospital or doctor's office. Connected health encompasses programs in telehealth, remote care and disease and lifestyle management, often leverages existing technologies such as connected devices using cellular networks and is associated with efforts to improve chronic care. However, there is an increasing blur between software capabilities and healthcare needs whereby technologists are now providing the solutions to support consumer wellness and provide the connectivity between patient data, information and decisions. This calls for new techniques to guide Connected Health solutions such as "design thinking" to support software developers in clearly identifying healthcare requirements, and extend and enrich traditional software requirements gathering techniques.

Remote patient monitoring (RPM) is a technology to enable monitoring of patients outside of conventional clinical settings, such as in the home or in a remote area, which may increase access to care and decrease healthcare delivery costs. RPM involves the constant remote care of patients by their physicians, often to track physical symptoms, chronic conditions, or post-hospitalization rehab.
Digital health is a discipline that includes digital care programs, technologies with health, healthcare, living, and society to enhance the efficiency of healthcare delivery and to make medicine more personalized and precise. It uses information and communication technologies to facilitate understanding of health problems and challenges faced by people receiving medical treatment and social prescribing in more personalised and precise ways. The definitions of digital health and its remits overlap in many ways with those of health and medical informatics.

The Binaytara Foundation (BTF) was established in 2007 by Dr. Binay Shah and wife Tara Shah with the goal of promoting health and education in underprivileged societies. The BTF is a Washington State nonprofit organization exempt from taxation pursuant to Section 501(c)(3) of the Internal Revenue Code. BTF has founded multiple programs in underdeveloped and developing countries to improve access to healthcare. Recent accomplishments include building a 25-bed cancer hospital in Nepal in 2018 and breaking ground on their new 200-bed facility in 2022.
Satmed is a satellite-based eHealth communications platform, in particular for provision of eHealth to remote, resource-poor areas of emerging and developing countries. It aims to provide services to non-governmental organisations (NGOs) that provide healthcare, education or health management services, governmental organisations that support regional development programs and humanitarian operations, and institutions such as medical universities, hospitals and health management institutions.

Sanjeev Arora, MD, MACP, FACG, an Indian American physician, is the founder and director of Project ECHO, a global tele-mentoring nonprofit dedicated to disseminating knowledge in rural and under-resourced communities.

Telehealth refers to the delivery of healthcare services through electronic communication methods, facilitating interactions between healthcare practitioners and patients using devices such as telephones, smartphones, tablets, and computers. It enables patients to engage with healthcare professionals through various means, including telephone calls, secure email, video conferencing, and secure messaging. Additionally, telehealth systems can be utilized by physicians for remote monitoring of patients in their homes.