Related Research Articles
Insulin resistance (IR) is a pathological condition in which cells either fail to respond normally to the hormone insulin or downregulate insulin receptors in response to hyperinsulinemia.

The glucose tolerance test is a medical test in which glucose is given and blood samples taken afterward to determine how quickly it is cleared from the blood. The test is usually used to test for diabetes, insulin resistance, impaired beta cell function, and sometimes reactive hypoglycemia and acromegaly, or rarer disorders of carbohydrate metabolism. In the most commonly performed version of the test, an oral glucose tolerance test (OGTT), a standard dose of glucose is ingested by mouth and blood levels are checked two hours later. Many variations of the GTT have been devised over the years for various purposes, with different standard doses of glucose, different routes of administration, different intervals and durations of sampling, and various substances measured in addition to blood glucose.

Hyperglycemia is a condition in which an excessive amount of glucose circulates in the blood plasma. This is generally a blood sugar level higher than 11.1 mmol/L (200 mg/dL), but symptoms may not start to become noticeable until even higher values such as 13.9–16.7 mmol/L (~250–300 mg/dL). A subject with a consistent fasting blood glucose range between ~5.6 and ~7 mmol/L is considered slightly hyperglycemic, and above 7 mmol/L is generally held to have diabetes. For diabetics, glucose levels that are considered to be too hyperglycemic can vary from person to person, mainly due to the person's renal threshold of glucose and overall glucose tolerance. On average, however, chronic levels above 10–12 mmol/L (180–216 mg/dL) can produce noticeable organ damage over time.
Drugs used in diabetes treat diabetes mellitus by decreasing the glucose level in the blood. With the exception of insulin, most GLP receptor agonists, and pramlintide, all are administered orally and are thus also called oral hypoglycemic agents or oral antihyperglycemic agents. There are different classes of hypoglycemic drugs, and their selection depends on the nature of diabetes, age, and situation of the person, as well as other factors.
Stress hyperglycemia is a medical term referring to transient elevation of the blood glucose due to the stress of illness. It usually resolves spontaneously, but must be distinguished from various forms of diabetes mellitus.

Reactive hypoglycemia, postprandial hypoglycemia, or sugar crash is a term describing recurrent episodes of symptomatic hypoglycemia occurring within four hours after a high carbohydrate meal in people with and without diabetes. The term is not necessarily a diagnosis since it requires an evaluation to determine the cause of the hypoglycemia.
Enteroglucagon is a peptide hormone derived from preproglucagon. It is a gastrointestinal hormone, secreted from mucosal cells primarily of the colon and terminal ileum. It consists of 37 amino acids. Enteroglucagon is released when fats and glucose are present in the small intestine; which decrease the motility to allow sufficient time for these nutrients to be absorbed.
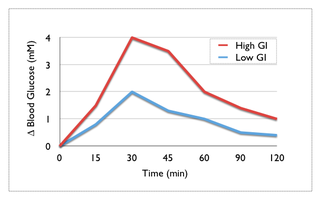
Many types of glucose tests exist and they can be used to estimate blood sugar levels at a given time or, over a longer period of time, to obtain average levels or to see how fast body is able to normalize changed glucose levels. Eating food for example leads to elevated blood sugar levels. In healthy people, these levels quickly return to normal via increased cellular glucose uptake which is primarily mediated by increase in blood insulin levels.

Exenatide, sold under the brand name Byetta and Bydureon among others, is a medication used to treat diabetes mellitus type 2. It is used together with diet, exercise, and potentially other antidiabetic medication. It is a treatment option after metformin and sulfonylureas. It is given by injection under the skin twice daily or once weekly.

Isomaltulose is a disaccharide carbohydrate composed of glucose and fructose. It is naturally present in honey and sugarcane extracts and is also produced industrially from table sugar (sucrose) and used as a sugar alternative.

Glucagon-like peptide-1 (GLP-1) is a 30- or 31-amino-acid-long peptide hormone deriving from the tissue-specific posttranslational processing of the proglucagon peptide. It is produced and secreted by intestinal enteroendocrine L-cells and certain neurons within the nucleus of the solitary tract in the brainstem upon food consumption. The initial product GLP-1 (1–37) is susceptible to amidation and proteolytic cleavage, which gives rise to the two truncated and equipotent biologically active forms, GLP-1 (7–36) amide and GLP-1 (7–37). Active GLP-1 protein secondary structure includes two α-helices from amino acid position 13–20 and 24–35 separated by a linker region.
Pioglitazone/metformin, sold under the brand name Actoplus Met among others, is a fixed-dose combination anti-diabetic medication used to improve glycemic control in adults with type 2 diabetes. It contains pioglitazone, a thiazolidinedione, and metformin, a biguanide.
Rabson–Mendenhall syndrome is a rare autosomal recessive disorder characterized by severe insulin resistance. The disorder is caused by mutations in the insulin receptor gene. Symptoms include growth abnormalities of the head, face and nails, along with the development of acanthosis nigricans. Treatment involves controlling blood glucose levels by using insulin and incorporating a strategically planned, controlled diet. Also, direct actions against other symptoms may be taken This syndrome usually affects children and has a prognosis of 1–2 years.

Prediabetes is a component of metabolic syndrome and is characterized by elevated blood sugar levels that fall below the threshold to diagnose diabetes mellitus. It usually does not cause symptoms but people with prediabetes often have obesity, dyslipidemia with high triglycerides and/or low HDL cholesterol, and hypertension. It is also associated with increased risk for cardiovascular disease (CVD). Prediabetes is more accurately considered an early stage of diabetes as health complications associated with type 2 diabetes often occur before the diagnosis of diabetes.
A postprandial glucose (PPG) test is a blood glucose test that determines the amount of glucose, in the plasma after a meal. The diagnosis is typically restricted to postprandial hyperglycemia due to lack of strong evidence of co-relation with a diagnosis of diabetes.
Complications of diabetes are secondary diseases that are a result of elevated blood glucose levels that occur in diabetic patients. These complications can be divided into two types: acute and chronic. Acute complications are complications that develop rapidly and can be exemplified as diabetic ketoacidosis (DKA), hyperglycemic hyperosmolar state (HHS), lactic acidosis (LA), and hypoglycemia. Chronic complications develop over time and are generally classified in two categories: microvascular and macrovascular. Microvascular complications include neuropathy, nephropathy, and retinopathy; while cardiovascular disease, stroke, and peripheral vascular disease are included in the macrovascular complications.

Gemigliptin (rINN), sold under the brand name Zemiglo, is an oral anti-hyperglycemic agent of the dipeptidyl peptidase-4 inhibitor class of drugs. Glucose lowering effects of DPP-4 inhibitors are mainly mediated by GLP-1 and gastric inhibitory polypeptide (GIP) incretin hormones which are inactivated by DPP-4.

Dulaglutide, sold under the brand name Trulicity among others, is a medication used for the treatment of type 2 diabetes in combination with diet and exercise. It is also approved in the United States for the reduction of major adverse cardiovascular events in adults with type 2 diabetes who have established cardiovascular disease or multiple cardiovascular risk factors. It is a once-weekly injection.

Omarigliptin (MK-3102) is a potent, long-acting oral antidiabetic drug of the DPP-4 inhibitor class used for once-weekly treatment of type 2 diabetes and currently under development by Merck & Co. It inhibits DPP-4 to increase incretin levels, which inhibit glucagon release, which in turn increases insulin secretion, decreases gastric emptying and decreases blood glucose levels.
References
- ↑ "Oxy- (sharp, pointed, keen; acidic, pungent) words: Oxymora to paroxysm, part 2 of 2".
- ↑ List of Greek and Latin roots in English
- ↑ Dorland (2011). Dorland's Illustrated Medical Dictionary E-Book: Dorland's Illustrated Medical Dictionary E-Book. Elsevier Health Sciences. p. 1008. ISBN 978-1-4557-0985-4.
- ↑ Takayoski Tobe; Mamoru Kouchi; Hiroshi Tanimura; Chiu Hsiung Huang Hyperglycemia After Gastrectomy as a Prediabetic State: Clinical Study of 100 Postgastrectomy Patients AMA Arch Surg. 1967; 94(6):836–840. http://archsurg.ama-assn.org/cgi/content/summary/94/6/836
- ↑ Nagoya J Med Sci. 1994 Mar;57(1-4):61–8. Glucose and insulin metabolism in patients with hyperthyroidism due to Graves' disease. Mano T, Kawakubo A, Yamamoto M. http://www.med.nagoya-u.ac.jp/medlib/nagoya_j_med_sci/5712/v57n12p61_68.pdf
- ↑ Lawrence, R.D.: Symptomless Glycosurias: Differentiation by Sugar Tolerance Tests, Med Clin N Amer 31:289, 1947
- ↑ Tobe T, Kouchi M, Tanimura H, Huang C. Hyperglycemia after gastrectomy as a prediabetic stateclinical study of 100 postgastrectomy patients. Arch Surg. 1967; 94(6):836–840.
- ↑ Gebhard, B.; Holst, J.J.; Biegelmayer, C.; Miholic, J. (1 September 2001). "Postprandial GLP-1, Norepinephrine, and Reactive Hypoglycemia in Dumping Syndrome". Digestive Diseases and Sciences. 46 (9): 1915–1923. doi:10.1023/A:1010635131228. ISSN 1573-2568.
- ↑ Yamamoto, Hiroshi; Mori, Tsuyoshi; Tsuchihashi, Hiroshi; Akabori, Hiroya; Naito, Hiroyuki; Tani, Tohru (1 December 2005). "A Possible Role of GLP-1 in the Pathophysiology of Early Dumping Syndrome". Digestive Diseases and Sciences. 50 (12): 2263–2267. doi:10.1007/s10620-005-3046-2. ISSN 1573-2568.
- ↑ The Journal of Clinical Endocrinology & Metabolism 1 December 2007 vol. 92 no. 12 4678–85 Patients with Neuroglycopenia after Gastric Bypass Surgery Have Exaggerated Incretin and Insulin Secretory Responses to a Mixed Meal. A. B. Goldfine, E. C. Mun, E. Devine, R. Bernier, M. Baz-Hecht, D. B. Jones, B. E. Schneider, J. J. Holst and M. E. Patti. http://jcem.endojournals.org/content/92/12/4678.full Archived 12 July 2013 at the Wayback Machine
- ↑ Journal of Endocrinology (1999) 160, 285–289 http://joe.endocrinology-journals.org/content/160/2/285.full.pdf