Related Research Articles

Dementia is a syndrome associated with many neurodegenerative diseases, characterized by a general decline in cognitive abilities that affects a person's ability to perform everyday activities. This typically involves problems with memory, thinking, behavior, and motor control. Aside from memory impairment and a disruption in thought patterns, the most common symptoms of dementia include emotional problems, difficulties with language, and decreased motivation. The symptoms may be described as occurring in a continuum over several stages. Dementia ultimately has a significant effect on the individual, their caregivers, and their social relationships in general. A diagnosis of dementia requires the observation of a change from a person's usual mental functioning and a greater cognitive decline than might be caused by the normal aging process.
The Glasgow Coma Scale (GCS) is a clinical scale used to reliably measure a person's level of consciousness after a brain injury.
The mini–mental state examination (MMSE) or Folstein test is a 30-point questionnaire that is used extensively in clinical and research settings to measure cognitive impairment. It is commonly used in medicine and allied health to screen for dementia. It is also used to estimate the severity and progression of cognitive impairment and to follow the course of cognitive changes in an individual over time; thus making it an effective way to document an individual's response to treatment. The MMSE's purpose has been not, on its own, to provide a diagnosis for any particular nosological entity.
The Abbreviated Mental Test score (AMTS) is a 10-point test for rapidly assessing elderly patients for the possibility of dementia. It was first used in 1972, and is now sometimes also used to assess for mental confusion and other cognitive impairments.
A pain scale measures a patient's pain intensity or other features. Pain scales are a common communication tool in medical contexts, and are used in a variety of medical settings. Pain scales are a necessity to assist with better assessment of pain and patient screening. Pain measurements help determine the severity, type, and duration of the pain, and are used to make an accurate diagnosis, determine a treatment plan, and evaluate the effectiveness of treatment. Pain scales are based on trust, cartoons (behavioral), or imaginary data, and are available for neonates, infants, children, adolescents, adults, seniors, and persons whose communication is impaired. Pain assessments are often regarded as "the 5th vital sign".
Nursing assessment is the gathering of information about a patient's physiological, psychological, sociological, and spiritual status by a licensed Registered Nurse. Nursing assessment is the first step in the nursing process. A section of the nursing assessment may be delegated to certified nurses aides. Vitals and EKG's may be delegated to certified nurses aides or nursing techs. It differs from a medical diagnosis. In some instances, the nursing assessment is very broad in scope and in other cases it may focus on one body system or mental health. Nursing assessment is used to identify current and future patient care needs. It incorporates the recognition of normal versus abnormal body physiology. Prompt recognition of pertinent changes along with the skill of critical thinking allows the nurse to identify and prioritize appropriate interventions. An assessment format may already be in place to be used at specific facilities and in specific circumstances.
OPQRST is a mnemonic initialism used by medical professionals to accurately discern reasons for a patient's symptoms and history in the event of an acute illness. It is specifically adapted to elicit symptoms of a possible heart attack. Each letter stands for an important line of questioning for the patient assessment. This is usually taken along with vital signs and the SAMPLE history and would usually be recorded by the person delivering the aid, such as in the "Subjective" portion of a SOAP note, for later reference.
The Clinical Dementia Rating or CDR is a numeric scale used to quantify the severity of symptoms of dementia.
As populations age, caring for people with dementia has become more common. Elderly caregiving may consist of formal care and informal care. Formal care involves the services of community and medical partners, while informal care involves the support of family, friends, and local communities. In most mild-to-medium cases of dementia, the caregiver is a spouse or an adult child. Over a period of time, more professional care in the form of nursing and other supportive care may be required medically, whether at home or in a long-term care facility. There is evidence to show that case management can improve care for individuals with dementia and the experience of their caregivers. Furthermore, case management may reduce overall costs and institutional care in the medium term. Millions of people living in the United States take care of a friend or family member with Alzheimer’s disease or a related dementia.
The visual analogue scale (VAS) is a psychometric response scale that can be used in questionnaires. It is a measurement instrument for subjective characteristics or attitudes that cannot be directly measured. When responding to a VAS item, respondents specify their level of agreement to a statement by indicating a position along a continuous line between two end points.
Wandering occurs when a person with dementia roams around and becomes lost or confused about their location. It is a common behavior that can cause great risk for the person, and is often the major priority for caregivers. It is estimated to be the most common form of disruption from people with dementia within institutions. Although it occurs in several types of dementia, wandering is especially common in people with Alzheimer's disease (AD). People with dementia often wander because they are stressed, looking for someone or something, attending to basic needs, engaging in past routines, or with visual-spatial problems. Other times, they may wander without aim at all.
The General Practitioner Assessment of Cognition (GPCOG) is a brief screening test for cognitive impairment introduced by Brodaty et al. in 2002. It was specifically developed for the use in the primary care setting.
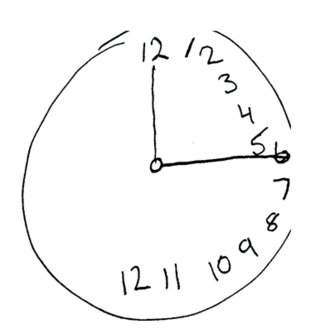
The Montreal Cognitive Assessment (MoCA) is a widely used screening assessment for detecting cognitive impairment. It was created in 1996 by Ziad Nasreddine in Montreal, Quebec. It was validated in the setting of mild cognitive impairment (MCI), and has subsequently been adopted in numerous other clinical settings. This test consists of 30 points and takes 10 minutes for the individual to complete. The original English version is performed in seven steps, which may change in some countries dependent on education and culture. The basics of this test include short-term memory, executive function, attention, focus, and more.
The Wechsler Memory Scale (WMS) is a neuropsychological test designed to measure different memory functions in a person. Anyone ages 16 to 90 is eligible to take this test. The current version is the fourth edition (WMS-IV) which was published in 2009 and which was designed to be used with the WAIS-IV. A person's performance is reported as five Index Scores: Auditory Memory, Visual Memory, Visual Working Memory, Immediate Memory, and Delayed Memory. The WMS-IV also incorporates an optional cognitive exam that helps to assess global cognitive functioning in people with suspected memory deficits or those who have been diagnosed with a various neural, psychiatric and/or developmental disorders. This may include conditions such as dementias or mild learning difficulties.
Pain is often regarded as the fifth vital sign in regard to healthcare because it is accepted now in healthcare that pain, like other vital signs, is an objective sensation rather than subjective. As a result nurses are trained and expected to assess pain.

The Wong–Baker Faces Pain Rating Scale is a pain scale that was developed by Donna Wong and Connie Baker. The scale shows a series of faces ranging from a happy face at 0, or "no hurt", to a crying face at 10, which represents "hurts like the worst pain imaginable". Based on the faces and written descriptions, the patient chooses the face that best describes their level of pain.
Pain stimulus is a technique used by medical personnel for assessing the consciousness level of a person who is not responding to normal interaction, voice commands or gentle physical stimuli. It forms one part of a number of neurological assessments, including the first aid based AVPU scale and the more medically based Glasgow Coma Scale.

The grimace scale (GS), sometimes called the grimace score, is a method of assessing the occurrence or severity of pain experienced by non-human animals according to objective and blinded scoring of facial expressions, as is done routinely for the measurement of pain in non-verbal humans. Observers score the presence or prominence of "facial action units" (FAU), e.g. Orbital Tightening, Nose Bulge, Ear Position and Whisker Change. These are scored by observing the animal directly in real-time, or post hoc from photographs or screen-grabs from videos. The facial expression of the animals is sometimes referred to as the pain face.
The Saint Louis University Mental Status (SLUMS) Exam is a brief screening assessment used to detect cognitive impairment. It was developed in 2006 at the Saint Louis University School of Medicine Division of Geriatric Medicine, in affiliation with a Veterans' Affairs medical center. The test was initially developed using a veteran population, but has since been adopted as a screening tool for any individual displaying signs of mild cognitive impairment. The intended population typically consists of individuals 60 years and above that display any signs of cognitive deficit. Unlike other widely-used cognitive screens, such as the Mini-Mental State Examination and Montreal Cognitive Assessment, the SLUMS is free to access and use by all healthcare professionals.
The Alzheimer's Disease Assessment Scale-Cognitive Subscale (ADAS-Cog) is a brief neuropsychological assessment used to assess the severity of cognitive symptoms of dementia. It is one of the most widely used cognitive scales in clinical trials and is considered to be the “gold standard” for assessing antidementia treatments.
References
- ↑ Development and Psychometric Evaluation of the Pain Assessment in Advanced Dementia (PAINAD) Scale [ unreliable source? ]
- ↑ "1 Pain Assessment in Advanced Dementia Scale (PAINAD)" (PDF). Archived from the original (PDF) on 2015-03-19. Retrieved 2014-05-16.