Pediatrics is the branch of medicine that involves the medical care of infants, children, adolescents, and young adults. In the United Kingdom, paediatrics covers many of their youth until the age of 18. The American Academy of Pediatrics recommends people seek pediatric care through the age of 21, but some pediatric subspecialists continue to care for adults up to 25. Worldwide age limits of pediatrics have been trending upward year after year. A medical doctor who specializes in this area is known as a pediatrician, or paediatrician. The word pediatrics and its cognates mean "healer of children", derived from the two Greek words: παῖς and ἰατρός. Pediatricians work in clinics, research centers, universities, general hospitals and children's hospitals, including those who practice pediatric subspecialties.

Skin is the layer of usually soft, flexible outer tissue covering the body of a vertebrate animal, with three main functions: protection, regulation, and sensation.

A burn is an injury to skin, or other tissues, caused by heat, cold, electricity, chemicals, friction, or ultraviolet radiation. Most burns are due to heat from hot liquids, solids, or fire. Burns occur mainly in the home or the workplace. In the home, risks are associated with domestic kitchens, including stoves, flames, and hot liquids. In the workplace, risks are associated with fire and chemical and electric burns. Alcoholism and smoking are other risk factors. Burns can also occur as a result of self-harm or violence between people (assault).

Fluid replacement or fluid resuscitation is the medical practice of replenishing bodily fluid lost through sweating, bleeding, fluid shifts or other pathologic processes. Fluids can be replaced with oral rehydration therapy (drinking), intravenous therapy, rectally such as with a Murphy drip, or by hypodermoclysis, the direct injection of fluid into the subcutaneous tissue. Fluids administered by the oral and hypodermic routes are absorbed more slowly than those given intravenously.
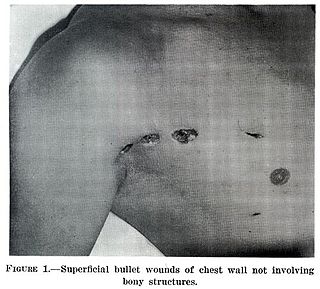
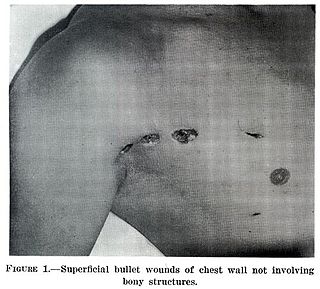
A wound is a rapid onset of injury that involves lacerated or punctured skin, or a contusion from blunt force trauma or compression. In pathology, a wound is an acute injury that damages the epidermis of the skin. To heal a wound, the body undertakes a series of actions collectively known as the wound healing process.

An injury is any physiological damage to living tissue caused by immediate physical stress. Injuries to humans can occur intentionally or unintentionally and may be caused by blunt trauma, penetrating trauma, burning, toxic exposure, asphyxiation, or overexertion. Injuries can occur in any part of the body, and different symptoms are associated with different injuries.

Skin grafting, a type of graft surgery, involves the transplantation of skin. The transplanted tissue is called a skin graft.
Grafting refers to a surgical procedure to move tissue from one site to another on the body, or from another creature, without bringing its own blood supply with it. Instead, a new blood supply grows in after it is placed. A similar technique where tissue is transferred with the blood supply intact is called a flap. In some instances, a graft can be an artificially manufactured device. Examples of this are a tube to carry blood flow across a defect or from an artery to a vein for use in hemodialysis.

A skin condition, also known as cutaneous condition, is any medical condition that affects the integumentary system—the organ system that encloses the body and includes skin, nails, and related muscle and glands. The major function of this system is as a barrier against the external environment.
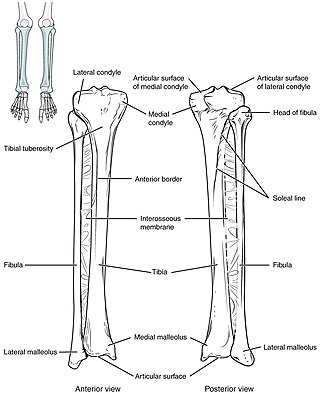
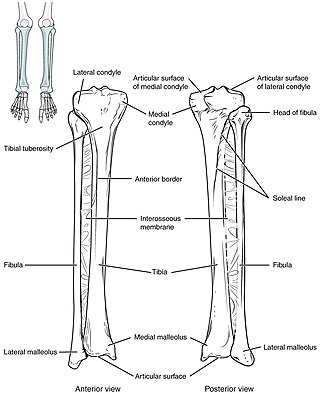
Intraosseous infusion (IO) is the process of injecting medications, fluids, or blood products directly into the marrow of a bone; this provides a non-collapsible entry point into the systemic venous system. The intraosseous infusion technique is used to provide fluids and medication when intravenous access is not available or not feasible. Intraosseous infusions allow for the administered medications and fluids to go directly into the vascular system. The IO route of fluid and medication administration is an alternative to the preferred intravascular route when the latter cannot be established promptly in emergent situations. Intraosseous infusions are used when people have compromised intravenous access and need immediate delivery of life-saving fluids and medications.

A radiation burn is a damage to the skin or other biological tissue and organs as an effect of radiation. The radiation types of greatest concern are thermal radiation, radio frequency energy, ultraviolet light and ionizing radiation.

Lymphangiomas are malformations of the lymphatic system characterized by lesions that are thin-walled cysts; these cysts can be macroscopic, as in a cystic hygroma, or microscopic. The lymphatic system is the network of vessels responsible for returning to the venous system excess fluid from tissues as well as the lymph nodes that filter this fluid for signs of pathogens. These malformations can occur at any age and may involve any part of the body, but 90% occur in children less than 2 years of age and involve the head and neck. These malformations are either congenital or acquired. Congenital lymphangiomas are often associated with chromosomal abnormalities such as Turner syndrome, although they can also exist in isolation. Lymphangiomas are commonly diagnosed before birth using fetal ultrasonography. Acquired lymphangiomas may result from trauma, inflammation, or lymphatic obstruction.

The human skin is the outer covering of the body and is the largest organ of the integumentary system. The skin has up to seven layers of ectodermal tissue guarding muscles, bones, ligaments and internal organs. Human skin is similar to most of the other mammals' skin, and it is very similar to pig skin. Though nearly all human skin is covered with hair follicles, it can appear hairless. There are two general types of skin, hairy and glabrous skin (hairless). The adjective cutaneous literally means "of the skin".
The Parkland formula, also known as Baxter formula, is a burn formula developed by Charles R. Baxter, used to estimate the amount of replacement fluid required for the first 24 hours in a burn patient so as to ensure the patient is hemodynamically stable. The milliliter amount of fluid required for the first 24 hours – usually Lactated Ringer's – is four times the product of the body weight and the burn percentage. The first half of the fluid is given within 8 hours from the burn incident, and the remaining over the next 16 hours. Only area covered by second-degree burns or greater is taken into consideration, as first-degree burns do not cause hemodynamically significant fluid shift to warrant fluid replacement.

Transdermal is a route of administration wherein active ingredients are delivered across the skin for systemic distribution. Examples include transdermal patches used for medicine delivery. The drug is administered in the form of a patch or ointment that delivers the drug into the circulation for systemic effect.

An escharotomy is a surgical procedure used to treat full-thickness (third-degree) circumferential burns. In full-thickness burns, both the epidermis and the dermis are destroyed along with sensory nerves in the dermis. The tough leathery tissue remaining after a full-thickness burn has been termed eschar. Following a full-thickness burn, as the underlying tissues are rehydrated, they become constricted due to the eschar's loss of elasticity, leading to impaired circulation distal to the wound. An escharotomy can be performed as a prophylactic measure as well as to release pressure, facilitate circulation and combat burn-induced compartment syndrome.

Artificial skin is a collagen scaffold that induces regeneration of skin in mammals such as humans. The term was used in the late 1970s and early 1980s to describe a new treatment for massive burns. It was later discovered that treatment of deep skin wounds in adult animals and humans with this scaffold induces regeneration of the dermis. It has been developed commercially under the name Integra and is used in massively burned patients, during plastic surgery of the skin, and in treatment of chronic skin wounds.

Fracture blisters occur on skin overlying a fractured bone, and fractures complicated by the development of overlying blisters remain a clinical dilemma in orthopedics.

An aerosol frostbite of the skin is an injury to the body caused by the pressurized gas within an aerosol spray cooling quickly, with the sudden drop in temperature sufficient to cause frostbite to the applied area. Medical studies have noted an increase of this practice, known as "frosting", in pediatric and teenage patients.

Alexander Burns Wallace (1906–1974) was a Scottish plastic surgeon. He was a founding member and president (1951) of the British Association of Plastic Surgeons, and the first editor of the British Journal of Plastic Surgery. In authorship he appears as A. B. Wallace.