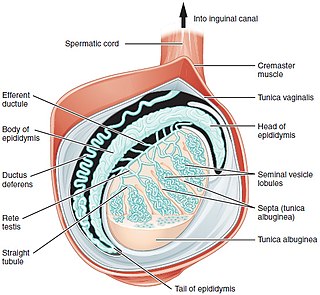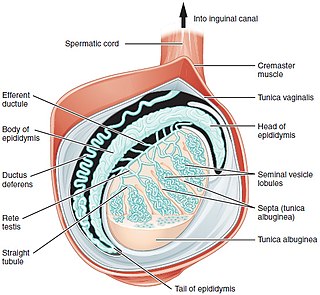
A testicle or testis is the male reproductive gland or gonad in all bilaterians, including humans. It is homologous to the female ovary. The functions of the testes are to produce both sperm and androgens, primarily testosterone. Testosterone release is controlled by the anterior pituitary luteinizing hormone, whereas sperm production is controlled both by the anterior pituitary follicle-stimulating hormone and gonadal testosterone.

Testicular torsion occurs when the spermatic cord twists, cutting off the blood supply to the testicle. The most common symptom in children is sudden, severe testicular pain. The testicle may be higher than usual in the scrotum and vomiting may occur. In newborns, pain is often absent and instead the scrotum may become discolored or the testicle may disappear from its usual place.

Testicular cancer is cancer that develops in the testicles, a part of the male reproductive system. Symptoms may include a lump in the testicle or swelling or pain in the scrotum. Treatment may result in infertility.

Cryptorchidism, also known as undescended testis, is the failure of one or both testes to descend into the scrotum. The word is from Greek κρυπτός 'hidden' and ὄρχις 'testicle'. It is the most common birth defect of the male genital tract. About 3% of full-term and 30% of premature infant boys are born with at least one undescended testis. However, about 80% of cryptorchid testes descend by the first year of life, making the true incidence of cryptorchidism around 1% overall. Cryptorchidism may develop after infancy, sometimes as late as young adulthood, but that is exceptional.

A hydrocele testis is an accumulation of clear fluid within the cavum vaginale, the potential space between the layers of the tunica vaginalis of the testicle. It is the most common form of hydrocele and is often referred to simply as a "hydrocele". A primary hydrocele testis causes a painless enlargement in the scrotum on the affected side and is thought to be due to the defective absorption of fluid secreted between the two layers of the tunica vaginalis. A secondary hydrocele is secondary to either inflammation or a neoplasm in the testis.

Epididymitis is a medical condition characterized by inflammation of the epididymis, a curved structure at the back of the testicle. Onset of pain is typically over a day or two. The pain may improve with raising the testicle. Other symptoms may include swelling of the testicle, burning with urination, or frequent urination. Inflammation of the testicle is commonly also present.

The cremasteric reflex is a superficial reflex observed in human males.
Orchitis is inflammation of the testicles. It can also involve swelling, pains and frequent infection, particularly of the epididymis, as in epididymitis. The term is from the Ancient Greek ὄρχις meaning "testicle"; same root as orchid.

Orchiopexy is a surgery to move and/or permanently fix a testicle into the scrotum. While orchiopexy typically describes the operation to surgically correct an undescended testicle, it is also used to resolve testicular torsion.

Spermatocele is a fluid-filled cyst that develops in the epididymis. The fluid is usually a clear or milky white color and may contain sperm. Spermatoceles are typically filled with spermatozoa and they can vary in size from several millimeters to many centimeters. Small spermatoceles are relatively common, occurring in an estimated 30 percent of males. They are generally not painful. However, some people may experience discomfort such as a dull pain in the scrotum from larger spermatoceles. They are not cancerous, nor do they cause an increased risk of testicular cancer. Additionally, unlike varicoceles, they do not reduce fertility.

Testicular atrophy is a medical condition in which one or both testicles diminish in size and may be accompanied by reduced testicular function. Testicular atrophy is not related to the temporary shrinkage of the surrounding scrotum, which might occur in response to cold temperature.

Polyorchidism is the incidence of more than two testicles. It is a very rare congenital disorder, with fewer than 200 cases reported in medical literature and six cases in veterinary literature.

A hydrocele is an accumulation of serous fluid in a body cavity. A hydrocele testis, the most common form of hydrocele, is the accumulation of fluids around a testicle. It is often caused by fluid collecting within a layer wrapped around the testicle, called the tunica vaginalis, which is derived from peritoneum. Provided there is no hernia present, it goes away without treatment in the first year. Although hydroceles usually develop in males, rare instances have been described in females in the canal of Nuck.

A hematocele is a collections of blood in a body cavity or potential space. The term most commonly refers to the collection of blood in the tunica vaginalis around the testes, known as a scrotal hematocele. Hematoceles can also occur in the abdominal cavity and other body cavities. Hematoceles are rare, making them harder to diagnose and treat. They are very common especially as slowly growing masses in the scrotum usually in men older than 50 years.

Testicular pain, also known as scrotal pain, occurs when part or all of either one or both testicles hurt. Pain in the scrotum is also often included. Testicular pain may be of sudden onset or of long duration.

The appendix testis is a vestigial remnant of the Müllerian duct, present on the upper pole of the testis and attached to the tunica vaginalis. It is present about 90% of the time and is homologous to the fallopian tubes in females.
Testicular trauma is an injury to one or both testicles. Types of injuries include blunt, penetrating and degloving.

Orchiectomy is a surgical procedure in which one or both testicles are removed. The surgery can be performed for various reasons:

Scrotalultrasound is a medical ultrasound examination of the scrotum. It is used in the evaluation of testicular pain, and can help identify solid masses.
Male genital examination is a physical examination of the genital in males to detect ailments and to assess sexual development, and is normally a component of an annual physical examination. The examination includes checking the penis, scrotum, and urethral meatus. A comprehensive assessment of the male genitals assesses the pubic hair based on Sexual Maturity Rating and the size of the testicles and penis. The exam can also be conducted to verify a person's age and biological sex. The genitourinary system can also be assessed as part of the male genital examination. During a genital examination, the doctor can detect any of the following: structural abnormalities, urethral opening abnormalities, problems related to not being circumcised, lumps, tumors, redness, excoriation, edema, lesions, swelling, cancer, hair-related issues, and many others. In some instances where a physical examination of the male genitals is not sufficient to diagnose an individual, then an internal genital examination using imaging or ultrasounds will be needed for further evaluation.