
Dentistry, also known as dental medicine and oral medicine, is the branch of medicine focused on the teeth, gums, and mouth. It consists of the study, diagnosis, prevention, management, and treatment of diseases, disorders, and conditions of the mouth, most commonly focused on dentition as well as the oral mucosa. Dentistry may also encompass other aspects of the craniofacial complex including the temporomandibular joint. The practitioner is called a dentist.

Trismus, commonly called lockjaw as associated with tetanus, is a condition of limited jaw mobility. It may be caused by spasm of the muscles of mastication or a variety of other causes. Temporary trismus occurs much more frequently than permanent trismus. It is known to interfere with eating, speaking, and maintaining proper oral hygiene. This interference, specifically with an inability to swallow properly, results in an increased risk of aspiration. In some instances, trismus presents with altered facial appearance. The condition may be distressing and painful. Examination and treatments requiring access to the oral cavity can be limited, or in some cases impossible, due to the nature of the condition itself.
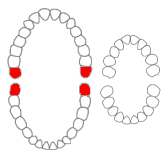
A third molar, commonly called wisdom tooth, is one of the three molars per quadrant of the human dentition. It is the most posterior of the three. The age at which wisdom teeth come through (erupt) is variable, but this generally occurs between late teens and early twenties. Most adults have four wisdom teeth, one in each of the four quadrants, but it is possible to have none, fewer, or more, in which case the extras are called supernumerary teeth. Wisdom teeth may get stuck (impacted) against other teeth if there is not enough space for them to come through normally. Impacted wisdom teeth are still sometimes removed for orthodontic treatment, believing that they move the other teeth and cause crowding, though this is not held anymore as true.
Oral and maxillofacial surgery is a surgical specialty focusing on reconstructive surgery of the face, facial trauma surgery, the oral cavity, head and neck, mouth, and jaws, as well as facial cosmetic surgery/facial plastic surgery including cleft lip and cleft palate surgery.

A mouthguard is a protective device for the mouth that covers the teeth and gums to prevent and reduce injury to the teeth, arches, lips and gums. An effective mouthguard is like a crash helmet for teeth and jaws. It also prevents the jaws coming together fully, thereby reducing the risk of jaw joint injuries and concussion. A mouthguard is most often used to prevent injury in contact sports, as a treatment for bruxism or TMD, or as part of certain dental procedures, such as tooth bleaching or sleep apnea treatment. Depending on application, it may also be called a mouth protector, mouth piece, gumshield, gumguard, nightguard, occlusal splint, bite splint, or bite plane. The dentists who specialise in sports dentistry fabricate mouthguards.

Alveolar osteitis, also known as dry socket, is inflammation of the alveolar bone. Classically, this occurs as a postoperative complication of tooth extraction.

Orthognathic surgery, also known as corrective jaw surgery or simply jaw surgery, is surgery designed to correct conditions of the jaw and lower face related to structure, growth, airway issues including sleep apnea, TMJ disorders, malocclusion problems primarily arising from skeletal disharmonies, other orthodontic dental bite problems that cannot be easily treated with braces, as well as the broad range of facial imbalances, disharmonies, asymmetries and malproportions where correction can be considered to improve facial aesthetics and self esteem.

Bone grafting is a surgical procedure that replaces missing bone in order to repair bone fractures that are extremely complex, pose a significant health risk to the patient, or fail to heal properly. Some small or acute fractures can be cured without bone grafting, but the risk is greater for large fractures like compound fractures.

A dental extraction is the removal of teeth from the dental alveolus (socket) in the alveolar bone. Extractions are performed for a wide variety of reasons, but most commonly to remove teeth which have become unrestorable through tooth decay, periodontal disease, or dental trauma, especially when they are associated with toothache. Sometimes impacted wisdom teeth cause recurrent infections of the gum (pericoronitis), and may be removed when other conservative treatments have failed. In orthodontics, if the teeth are crowded, healthy teeth may be extracted to create space so the rest of the teeth can be straightened.

Pericoronitis is inflammation of the soft tissues surrounding the crown of a partially erupted tooth, including the gingiva (gums) and the dental follicle. The soft tissue covering a partially erupted tooth is known as an operculum, an area which can be difficult to access with normal oral hygiene methods. The hyponym operculitis technically refers to inflammation of the operculum alone.

Maxillary sinus floor augmentation is a surgical procedure which aims to increase the amount of bone in the posterior maxilla, in the area of the premolar and molar teeth, by lifting the lower Schneiderian membrane and placing a bone graft.
Dental pertains to the teeth, including dentistry. Topics related to the dentistry, the human mouth and teeth include:

Facial trauma, also called maxillofacial trauma, is any physical trauma to the face. Facial trauma can involve soft tissue injuries such as burns, lacerations and bruises, or fractures of the facial bones such as nasal fractures and fractures of the jaw, as well as trauma such as eye injuries. Symptoms are specific to the type of injury; for example, fractures may involve pain, swelling, loss of function, or changes in the shape of facial structures.

Medication-related osteonecrosis of the jaw is progressive death of the jawbone in a person exposed to a medication known to increase the risk of disease, in the absence of a previous radiation treatment. It may lead to surgical complication in the form of impaired wound healing following oral and maxillofacial surgery, periodontal surgery, or endodontic therapy.

Mandibular fracture, also known as fracture of the jaw, is a break through the mandibular bone. In about 60% of cases the break occurs in two places. It may result in a decreased ability to fully open the mouth. Often the teeth will not feel properly aligned or there may be bleeding of the gums. Mandibular fractures occur most commonly among males in their 30s.

Osteoradionecrosis (ORN) is a serious complication of radiation therapy in cancer treatment where radiated bone becomes necrotic and exposed. ORN occurs most commonly in the mouth during the treatment of head and neck cancer, and can arise over 5 years after radiation. Common signs and symptoms include pain, difficulty chewing, trismus, mouth-to-skin fistulas and non-healing ulcers.

Impacted wisdom teeth is a condition where the third molars are prevented from erupting into the mouth. This can be caused by a physical barrier, such as other teeth, or when the tooth is angled away from a vertical position. Completely unerupted wisdom teeth usually result in no symptoms, although they can sometimes develop cysts or neoplasms. Partially erupted wisdom teeth can develop cavities or pericoronitis. Removal of impacted wisdom teeth is advised in the case of certain pathologies, such as nonrestorable caries or cysts.

Frank Hölzle is a German surgeon. He is a professor of oral and maxillofacial surgery at the RWTH Aachen University. He is chairman and head of the Department of Oral and Maxillofacial Surgery. Hölzle is known for his work in the fields of plastic facial reconstruction with a focus on micro surgery. He is also specialised for the treatment of tumor diseases in the head and neck region, and of malformations like cleft lip and palate.
Hugo Obwegeser was an Austrian Oral and Maxillo-Facial Surgeon and Plastic Surgeon who is known as the father of the modern orthognathic surgery. In his publication of 1970, he was the first surgeon to describe the simultaneous procedure which involved surgeries of both Maxilla and Mandible involving Le Fort I and Bilateral Sagittal Split Osteotomy technique.
Pradeep Adatrow is an Indian-American dental educator, researcher and clinician. He is a board certified Periodontist and Prosthodontists in the United States. He is an Associate Professor at the University of Tennessee.




















