Related Research Articles

Anesthesia or anaesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.

Anesthesiology or anaesthesiology is the medical specialty concerned with the total perioperative care of patients before, during and after surgery. It encompasses anesthesia, intensive care medicine, critical emergency medicine, and pain medicine. A physician specialized in anesthesiology is called an anesthesiologist, anaesthesiologist, or anaesthetist, depending on the country. In some countries, the terms are synonymous, while in other countries, they refer to different positions and anesthetist is only used for non-physicians, such as nurse anesthetists.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true anaesthesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
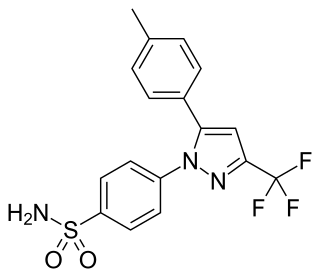
Celecoxib, sold under the brand name Celebrex among others, is a COX-2 inhibitor and nonsteroidal anti-inflammatory drug (NSAID). It is used to treat the pain and inflammation in osteoarthritis, acute pain in adults, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, painful menstruation, and juvenile rheumatoid arthritis. It may also be used to decrease the risk of colorectal adenomas in people with familial adenomatous polyposis. It is taken by mouth. Benefits are typically seen within an hour.
Awareness under anesthesia, also referred to as intraoperative awareness or accidental awareness during general anesthesia (AAGA), is a rare complication of general anesthesia where patients regain varying levels of consciousness during their surgical procedures. While anesthesia awareness is possible without resulting in any long-term memory of the experience, it is also possible for victims to have awareness with explicit recall, where they can remember the events related to their surgery.
Cyclooxygenase-2 inhibitors, also known as coxibs, are a type of nonsteroidal anti-inflammatory drug (NSAID) that directly target cyclooxygenase-2 (COX-2), an enzyme responsible for inflammation and pain. Targeting selectivity for COX-2 reduces the risk of peptic ulceration and is the main feature of celecoxib, rofecoxib, and other members of this drug class.

A nurse anesthetist is an advanced practice nurse who administers anesthesia for surgery or other medical procedures. Nurse anesthetists (NA's) administer or participate in administration of anesthesia services in 107 countries, working with or without anesthesiologists. Because of different historical backgrounds, anesthetist responsibilities and roles vary widely between countries. Depending on the locality, their role may be limited to intraoperative care during anesthesia itself or may also extend before and after. The International Federation of Nurse Anesthetists was established in 1989 as a forum for developing standards of education, practice, and a code of ethics.
Veterinary anesthesia is a specialization in the veterinary medicine field dedicated to the proper administration of anesthetic agents to non-human animals to control their consciousness during procedures. A veterinarian or a Registered Veterinary Technician administers these drugs to minimize stress, destructive behavior, and the threat of injury to both the patient and the doctor. The duration of the anesthesia process goes from the time before an animal leaves for the visit to the time after the animal reaches home after the visit, meaning it includes care from both the owner and the veterinary staff. Generally, anesthesia is used for a wider range of circumstances in animals than in people not only due to their inability to cooperate with certain diagnostic or therapeutic procedures, but also due to their species, breed, size, and corresponding anatomy. Veterinary anesthesia includes anesthesia of the major species: dogs, cats, horses, cattle, sheep, goats, and pigs, as well as all other animals requiring veterinary care such as birds, pocket pets, and wildlife.
Harold Randall Griffith was a Canadian anesthesiologist and a leader in the fields of anesthesiology.
Cardiothoracic anesthesiology is a subspeciality of the medical practice of anesthesiology, devoted to the preoperative, intraoperative, and postoperative care of adult and pediatric patients undergoing cardiothoracic surgery and related invasive procedures.
Geriatric anesthesia is the branch of medicine that studies anesthesia approach in elderly.
Neurosurgical anesthesiology, neuroanesthesiology, or neurological anesthesiology is a subspecialty of anesthesiology devoted to the total perioperative care of patients before, during, and after neurological surgeries, including surgeries of the central (CNS) and peripheral nervous systems (PNS). The field has undergone extensive development since the 1960s correlating with the ability to measure intracranial pressure (ICP), cerebral blood flow (CBF), and cerebral metabolic rate (CMR).

Throughout recorded history, attempts at producing a state of general anesthesia can be traced back to the writings of ancient Sumerians, Babylonians, Assyrians, Egyptians, Indians, and Chinese. Despite significant advances in anatomy and surgical technique during the Renaissance, surgery remained a last-resort treatment largely due to the pain associated with it. However, scientific discoveries in the late 18th and early 19th centuries paved the way for the development of modern anesthetic techniques.
Joachim Boldt is a German anesthesiologist who fabricated or falsified data, including those reporting clinical trial results.
Certified anesthesiologist assistants (CAAs) are master’s degree level non-physician anesthesia care providers. CAAs are members of the anesthesia care team as described by the American Society of Anesthesiologists (ASA). This designation must be disambiguated from the Certified Clinical Anesthesia Assistant (CCAA) designation conferred by the Canadian Society of Respiratory Therapists. All CAAs possess a baccalaureate degree, and complete an intensive didactic and clinical program at a postgraduate level. CAAs are trained in the delivery and maintenance of most types of anesthesia care as well as advanced patient monitoring techniques. The goal of CAA education is to guide the transformation of student applicants into competent clinicians.
The following outline is provided as an overview of and topical guide to anesthesia:
Yoshitaka Fujii is a Japanese researcher in anesthesiology, who in 2012 was found to have fabricated data in at least 219 scientific papers, of which 183 have been retracted.
Obstetric anesthesia or obstetric anesthesiology, also known as ob-gyn anesthesia or ob-gyn anesthesiology, is a sub-specialty of anesthesiology that provides peripartum pain relief (analgesia) for labor and anesthesia for cesarean deliveries ('C-sections').

Alex Bekker is a physician, author and academic. He is a professor and chair at the Department of Anesthesiology, Rutgers New Jersey Medical School. He is also professor at the Department of Physiology, Pharmacology & Neurosciences. He serves as the Chief of Anesthesiology Service at the University Hospital in Newark.
Alex Macario is an American anesthesiologist, academic and author. He is a vice-chair for education, a professor in the Department of Anesthesiology, Perioperative and Pain Medicine, and program director for the anesthesiology residency at Stanford University School of Medicine.
References
- 1 2 3 4 5 6 "A Medical Madoff: Anesthesiologist Faked Data in 21 Studies", Scientific American , March 10, 2009, retrieved December 27, 2015
- ↑ "Fraud Case Stuns Anesthesiologists Post-op Pain Expert Fabricated Years of Data", Anesthesiology News, vol. 35, no. 4, April 2009, retrieved 27 December 2015
- 1 2 Harris, Gardiner (March 11, 2009), "Doctor Admits Pain Studies Were Frauds, Hospital Says", The New York Times , retrieved December 27, 2015
- 1 2 3 "Fraud Case Rocks Anesthesiology Community", Anesthesiology News, March 2009
- 1 2 3 4 Doctor accused of faking studies; His work dealt with pain drugs, Boston Globe, March 11, 2009
- 1 2 Mass. doctor accused of fabricating pain studies, Associated Press, March 11, 2009
- 1 2 3 Top Pain Scientist Fabricated Data in Studies, Hospital Says, Wall Street Journal, March 11, 2009
- ↑ "Retraction Notice", Steven L. Shafer, Anesthesia and Analgesia , 20 February 2009
- ↑ Dr. Scott Reuben, former chief of acute pain at Baystate Medical Center in Springfield, pleads guilty to health-care fraud. The Republican, January 15, 2010
- ↑ Scott Reuben, a former Baystate doctor who faked research, sentenced to 6 months for health care fraud, The Republican, June 24, 2010
- ↑ Anesthesiologist sentenced on health care fraud charge Archived 2011-05-31 at the Wayback Machine . United States Attorney for the District of Massachusetts, June 24, 2010
- ↑ Scott S. Reuben: Debarment Order (FDA)
- 1 2 Marret; et al. (Dec 2009). "lessons from the Reuben case". Anesthesiology. 111 (6): 1279–89. doi: 10.1097/ALN.0b013e3181c14c3d . PMID 19934873.
- ↑ Moore, R. A.; Derry, S.; McQuay, H. J. (17 March 2010). "Fraud or flawed: adverse impact of fabricated or poor quality research". Anaesthesia. 65 (4): 327–330. doi: 10.1111/j.1365-2044.2010.06295.x . PMID 20402871.