Pediatrics is the branch of medicine that involves the medical care of infants, children, adolescents, and young adults. In the United Kingdom, paediatrics covers many of their youth until the age of 18. The American Academy of Pediatrics recommends people seek pediatric care through the age of 21, but some pediatric subspecialists continue to care for adults up to 25. Worldwide age limits of pediatrics have been trending upward year after year. A medical doctor who specializes in this area is known as a pediatrician, or paediatrician. The word pediatrics and its cognates mean "healer of children", derived from the two Greek words: παῖς and ἰατρός. Pediatricians work in clinics, research centers, universities, general hospitals and children's hospitals, including those who practice pediatric subspecialties.

Intensive care medicine, also called critical care medicine, is a medical specialty that deals with seriously or critically ill patients who have, are at risk of, or are recovering from conditions that may be life-threatening. It includes providing life support, invasive monitoring techniques, resuscitation, and end-of-life care. Doctors in this specialty are often called intensive care physicians, critical care physicians, or intensivists.

Anesthesiology, anaesthesiology, or anaesthesia is the medical specialty concerned with the total perioperative care of patients before, during and after surgery. It encompasses anesthesia, intensive care medicine, critical emergency medicine, and pain medicine. A physician specialized in anesthesiology is called an anesthesiologist, anaesthesiologist, or anaesthetist, depending on the country. In some countries, the terms are synonymous, while in other countries they refer to different positions, and anesthetist is only used for non-physicians, such as nurse anesthetists.
The American Academy of Pediatrics (AAP) is the largest professional association of pediatricians in the United States. It is headquartered in DuPage County, Illinois, and maintains an office in Washington, D.C. The AAP has published hundreds of policy statements, ranging from advocacy issues to practice recommendations.
Systemic inflammatory response syndrome (SIRS) is an inflammatory state affecting the whole body. It is the body's response to an infectious or noninfectious insult. Although the definition of SIRS refers to it as an "inflammatory" response, it actually has pro- and anti-inflammatory components.
An induced coma – also known as a medically induced coma (MIC), barbiturate-induced coma, or drug-induced coma – is a temporary coma brought on by a controlled dose of an anesthetic drug, often a barbiturate such as pentobarbital or thiopental. Other intravenous anesthetic drugs such as midazolam or propofol may be used.

A neonatal intensive care unit (NICU), also known as an intensive care nursery (ICN), is an intensive care unit (ICU) specializing in the care of ill or premature newborn infants. The NICU is divided into several areas, including a critical care area for babies who require close monitoring and intervention, an intermediate care area for infants who are stable but still require specialized care, and a step down unit where babies who are ready to leave the hospital can receive additional care before being discharged.
Patient safety is a discipline that emphasizes safety in health care through the prevention, reduction, reporting and analysis of error and other types of unnecessary harm that often lead to adverse patient events. The frequency and magnitude of avoidable adverse events, often known as patient safety incidents, experienced by patients was not well known until the 1990s, when multiple countries reported significant numbers of patients harmed and killed by medical errors. Recognizing that healthcare errors impact 1 in every 10 patients around the world, the World Health Organization (WHO) calls patient safety an endemic concern. Indeed, patient safety has emerged as a distinct healthcare discipline supported by an immature yet developing scientific framework. There is a significant transdisciplinary body of theoretical and research literature that informs the science of patient safety with mobile health apps being a growing area of research.
Adolescent medicine also known as adolescent and young adult medicine is a medical subspecialty that focuses on care of patients who are in the adolescent period of development. This period begins at puberty and lasts until growth has stopped, at which time adulthood begins. Typically, patients in this age range will be in the last years of middle school up until college graduation. In developed nations, the psychosocial period of adolescence is extended both by an earlier start, as the onset of puberty begins earlier, and a later end, as patients require more years of education or training before they reach economic independence from their parents.

An intensive care unit (ICU), also known as an intensive therapy unit or intensive treatment unit (ITU) or critical care unit (CCU), is a special department of a hospital or health care facility that provides intensive care medicine.

Neurocritical care is a medical field that treats life-threatening diseases of the nervous system and identifies, prevents, and treats secondary brain injury.

A pediatric intensive care unit, usually abbreviated to PICU, is an area within a hospital specializing in the care of critically ill infants, children, teenagers, and young adults aged 0-21. A PICU is typically directed by one or more pediatric intensivists or PICU consultants and staffed by doctors, nurses, and respiratory therapists who are specially trained and experienced in pediatric intensive care. The unit may also have nurse practitioners, physician assistants, physiotherapists, social workers, child life specialists, and clerks on staff, although this varies widely depending on geographic location. The ratio of professionals to patients is generally higher than in other areas of the hospital, reflecting the acuity of PICU patients and the risk of life-threatening complications. Complex technology and equipment is often in use, particularly mechanical ventilators and patient monitoring systems. Consequently, PICUs have a larger operating budget than many other departments within the hospital.
The Emergency Medical Services for Children (EMSC) program is a US federal government health initiative. It is administered by the U.S. Department of Health and Human Services’ Health Resources and Services Administration (HRSA), and the Maternal and Child Health Bureau (MCHB). Its aim is to reduce child and youth disability and death due to severe illness or injury by increasing awareness among health professionals, provider and planners and the general public of the special needs of children receiving emergency medical care.
Robert (Bob) Bartlett is an American physician and medical researcher who is credited with developing a lifesaving heart-lung technology known as extracorporeal membrane oxygenation (ECMO). He is an emeritus professor of surgery at the University of Michigan Medical School.
Pediatric early warning signs (PEWS) are clinical manifestations that indicate rapid deterioration in pediatric patients, infancy to adolescence. A PEWS score or PEWS system refers to assessment tools that incorporate the clinical manifestations that have the greatest impact on patient outcome.

Robert D. Truog is an American bioethicist and pediatrician. He is the Frances Glessner Lee Professor of Medical Ethics, Anaesthesiology & Pediatrics at Harvard Medical School, where he is also the Director of the Center for Bioethics. He also practices in the pediatric intensive care unit at Boston Children’s Hospital, where he previously served as chair of the Division of Critical Care Medicine.

Critical emergency medicine (CREM) refers to the acute medical care of patients who have medical emergencies that pose an immediate threat to life, irrespective of location. In particular, the term is used to describe the role of anaesthesiologists in providing such care.
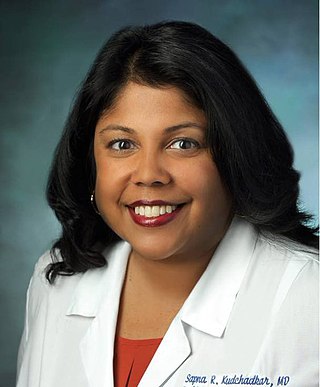
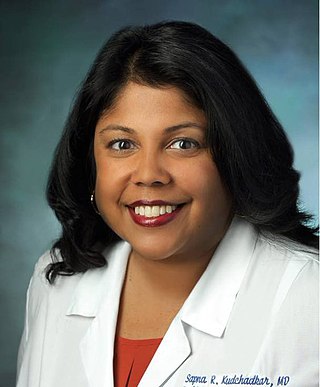
Sapna Ravi Kudchadkar is an American critical care physician and anesthesiologist. She is an Associate professor of anesthesiology and critical care medicine, pediatrics and physical medicine and rehabilitation at the Johns Hopkins School of Medicine. In 2022, she was appointed Vice Chair of Pediatric Anesthesiology and Critical Care Medicine at Johns Hopkins as well as Anesthesiologist-in-Chief of the Johns Hopkins Charlotte R. Bloomberg Children's Center.
The Holliday-Segar formula is a formula to help approximate water and caloric loss using a patient's body weight. Primarily aimed at pediatric patients, the Holliday-Segar formula is the most commonly used estimate of daily caloric requirements. To date, the formula continues to be recommended in the current clinical practice guidelines of the American Academy of Pediatrics, American Society of Parenteral and Enteral Nutrition, and National Health Service. Developed in 1957 by Drs. Malcolm A. Holliday and William E. Segar while at the Indiana University School of Medicine, the researchers concluded a non-linear relationship between energy expenditure and weight alone to determine fluid requirements.
Vinay M. Nadkarni is an American pediatric critical care physician. He is a Professor of Anesthesiology and Critical Care at the Hospital of the University of Pennsylvania and the Medical Director of the Center for Simulation, Advanced Education and Innovation at the Children's Hospital of Philadelphia (CHOP). Nadkarni also holds the institution’s Endowed Chair in Pediatric Critical Care Medicine and is a Fellow of the American College of Critical Care Medicine, the American Academy of Pediatrics, and the American Heart Association.