Related Research Articles
A transient ischemic attack (TIA), commonly known as a mini-stroke, is a brief episode of neurological dysfunction caused by loss of blood flow (ischemia) in the brain, spinal cord, or retina, without tissue death (infarction). TIAs have the same underlying mechanism as ischemic strokes. Both are caused by a disruption in blood flow to the brain, or cerebral blood flow (CBF). The definition of TIA was classically based on duration of neurological symptoms. The current widely accepted definition is called "tissue-based" because it is based on imaging, not time. The American Heart Association and the American Stroke Association (AHA/ASA) now define TIA as a brief episode of neurological dysfunction with a vascular cause, with clinical symptoms typically lasting less than one hour, and without evidence of infarction on imaging.

Angina, also known as angina pectoris, is chest pain or pressure, usually due to insufficient blood flow to the heart muscle (myocardium).

Hypertension, also known as high blood pressure (HBP), is a long-term medical condition in which the blood pressure in the arteries is persistently elevated. High blood pressure typically does not cause symptoms. Long-term high blood pressure, however, is a major risk factor for stroke, coronary artery disease, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia.

Thrombolysis, also called fibrinolytic therapy, is the breakdown (lysis) of blood clots formed in blood vessels, using medication. It is used in ST elevation myocardial infarction, stroke, and in cases of severe venous thromboembolism.
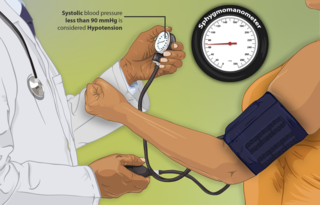
Hypotension is low blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood. Blood pressure is indicated by two numbers, the systolic blood pressure and the diastolic blood pressure, which are the maximum and minimum blood pressures, respectively. A systolic blood pressure of less than 90 millimeters of mercury or diastolic of less than 60 mm Hg is generally considered to be hypotension. Different numbers apply to children. However, in practice, blood pressure is considered too low only if noticeable symptoms are present.
Antihypertensives are a class of drugs that are used to treat hypertension. Antihypertensive therapy seeks to prevent the complications of high blood pressure, such as stroke and myocardial infarction. Evidence suggests that reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34%, of ischaemic heart disease by 21%, and reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease. There are many classes of antihypertensives, which lower blood pressure by different means. Among the most important and most widely used medications are thiazide diuretics, calcium channel blockers, ACE inhibitors, angiotensin II receptor antagonists (ARBs), and beta blockers.

A cardiac stress test is a cardiological test that measures the heart's ability to respond to external stress in a controlled clinical environment. The stress response is induced by exercise or by intravenous pharmacological stimulation.

Coronary thrombosis is defined as the formation of a blood clot inside a blood vessel of the heart. This blood clot may then restrict blood flow within the heart, leading to heart tissue damage, or a myocardial infarction, also known as a heart attack.
The Killip classification is a system used in individuals with an acute myocardial infarction, taking into account physical examination and the development of heart failure in order to predict and stratify their risk of mortality. Individuals with a low Killip class are less likely to die within the first 30 days after their myocardial infarction than individuals with a high Killip class.

Acute coronary syndrome (ACS) is a syndrome due to decreased blood flow in the coronary arteries such that part of the heart muscle is unable to function properly or dies. The most common symptom is centrally located chest pain, often radiating to the left shoulder or angle of the jaw, crushing, central and associated with nausea and sweating. Many people with acute coronary syndromes present with symptoms other than chest pain, particularly women, older people, and people with diabetes mellitus.

A hypertensive emergency is very high blood pressure with potentially life-threatening symptoms and signs of acute damage to one or more organ systems. It is different from a hypertensive urgency by this additional evidence for impending irreversible hypertension-mediated organ damage (HMOD). Blood pressure is often above 200/120 mmHg, however there are no universally accepted cutoff values. Signs of organ damage will be discussed below.
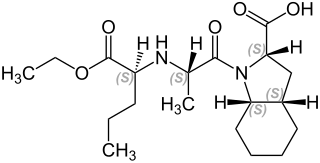
Perindopril is a medication used to treat high blood pressure, heart failure, or stable coronary artery disease.
In medicine, systolic hypertension is defined as an elevated systolic blood pressure (SBP). If the systolic blood pressure is elevated (>140) with a normal (<90) diastolic blood pressure (DBP), it is called "isolated systolic hypertension".
The Thrombolysis In Myocardial Infarction, or TIMI Study Group, is an Academic Research Organization (ARO) affiliated with Brigham and Women's Hospital and Harvard Medical School dedicated to advancing the knowledge and care of patients suffering from cardiovascular disease. The TIMI Study Group provides robust expertise in the key aspects of a clinical trial, including academic leadership, global trial management, biostatistics, clinical event adjudication, safety desk, medical hotline, and core laboratories. The group has its headquarters in Boston, Massachusetts.
Naproxcinod (nitronaproxen) is a nonsteroidal anti-inflammatory drug (NSAID) developed by the French pharmaceutical company NicOx. It is a derivative of naproxen with a nitroxybutyl ester to allow it to also act as a nitric oxide (NO) donor. This second mechanism of action makes naproxcinod the first in a new class of drugs, the cyclooxygenase inhibiting nitric oxide donators (CINODs), that are hoped to produce similar analgesic efficacy to traditional NSAIDs, but with less gastrointestinal and cardiovascular side effects.

Clevidipine is a dihydropyridine calcium channel blocker indicated for the reduction of blood pressure when oral therapy is not feasible or not desirable. Clevidipine is used IV only and practioners titrate this drug to lower blood pressure. It has a half-life of approximately one minute. It is rapidly inactivated by esterases.

A myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow decreases or stops to the coronary artery of the heart, causing damage to the heart muscle. The most common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck or jaw. Often it occurs in the center or left side of the chest and lasts for more than a few minutes. The discomfort may occasionally feel like heartburn. Other symptoms may include shortness of breath, nausea, feeling faint, a cold sweat or feeling tired. About 30% of people have atypical symptoms. Women more often present without chest pain and instead have neck pain, arm pain or feel tired. Among those over 75 years old, about 5% have had an MI with little or no history of symptoms. An MI may cause heart failure, an irregular heartbeat, cardiogenic shock or cardiac arrest.

Management of acute coronary syndrome is targeted against the effects of reduced blood flow to the afflicted area of the heart muscle, usually because of a blood clot in one of the coronary arteries, the vessels that supply oxygenated blood to the myocardium. This is achieved with urgent hospitalization and medical therapy, including drugs that relieve chest pain and reduce the size of the infarct, and drugs that inhibit clot formation; for a subset of patients invasive measures are also employed. Basic principles of management are the same for all types of acute coronary syndrome. However, some important aspects of treatment depend on the presence or absence of elevation of the ST segment on the electrocardiogram, which classifies cases upon presentation to either ST segment elevation myocardial infarction (STEMI) or non-ST elevation acute coronary syndrome (NST-ACS); the latter includes unstable angina and non-ST elevation myocardial infarction (NSTEMI). Treatment is generally more aggressive for STEMI patients, and reperfusion therapy is more often reserved for them. Long-term therapy is necessary for prevention of recurrent events and complications.
Permissive hypotension or hypotensive resuscitation is the use of restrictive fluid therapy, specifically in the trauma patient, that increases systemic blood pressure without reaching normotension. The goal blood pressure for these patients is a mean arterial pressure of 40-50mmHg or a systolic blood pressure less than or equal to 80. This goes along with certain clinical criteria. Following traumatic injury some patients experience hypotension that is usually due to blood loss (hemorrhage) but can be due to other causes as well. In the past, physicians were very aggressive with fluid resuscitation to try to bring the blood pressure to normal values. Recent studies have found that there is some benefit to allowing specific patients to experience some degree of hypotension in certain settings. This concept does not exclude therapy by means of i.v. fluid, inotropes or vasopressors, the only restriction is to avoid completely normalizing blood pressure in a context where blood loss may be enhanced. When a person starts to bleed the body starts a natural coagulation process that eventually stops the bleed. Issues with fluid resuscitation without control of bleeding is thought to be secondary to dislodgement of the thrombus that is helping to control further bleeding. Thrombus dislodgement was found to occur at a systolic pressure greater than 80mm Hg. In addition, fluid resuscitation will dilute coagulation factors that help form and stabilize a clot, hence making it harder for the body to use its natural mechanisms to stop the bleeding. These factors are aggravated by hypothermia.
Hypertension is managed using lifestyle modification and antihypertensive medications. Hypertension is usually treated to achieve a blood pressure of below 140/90 mmHg to 160/100 mmHg. According to one 2003 review, reduction of the blood pressure by 5 mmHg can decrease the risk of stroke by 34%, of ischaemic heart disease by 21%, and reduce the likelihood of dementia, heart failure, and mortality from cardiovascular disease.
References
- 1 2 3 4 5 6 7 8 9 10 11 Wright JT, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, et al. (November 2015). "A Randomized Trial of Intensive versus Standard Blood-Pressure Control". The New England Journal of Medicine. 373 (22): 2103–2116. doi:10.1056/nejmoa1511939. PMC 4689591 . PMID 26551272.
- ↑ Egan BM, Li J, Wagner CS (August 2016). "Systolic Blood Pressure Intervention Trial (SPRINT) and Target Systolic Blood Pressure in Future Hypertension Guidelines". Hypertension. 68 (2): 318–323. doi:10.1161/hypertensionaha.116.07575. PMID 27354422. S2CID 446300.
- ↑ Ruiz-Hurtado G, Banegas JR, Sarafidis PA, Volpe M, Williams B, Ruilope LM (September 2017). "Has the SPRINT trial introduced a new blood-pressure goal in hypertension?". Nature Reviews. Cardiology. 14 (9): 560–566. doi:10.1038/nrcardio.2017.74. PMID 28492286. S2CID 23707851.