Tetraplegia, also known as quadriplegia, is defined as the dysfunction or loss of motor and/or sensory function in the cervical area of the spinal cord. A loss of motor function can present as either weakness or paralysis leading to partial or total loss of function in the arms, legs, trunk, and pelvis; paraplegia is similar but affects the thoracic, lumbar, and sacral segments of the spinal cord and arm function is retained. The paralysis may be flaccid or spastic. A loss of sensory function can present as an impairment or complete inability to sense light touch, pressure, heat, pinprick/pain, and proprioception. In these types of spinal cord injury, it is common to have a loss of both sensation and motor control.

The median nerve is a nerve in humans and other animals in the upper limb. It is one of the five main nerves originating from the brachial plexus.

The anterior cruciate ligament (ACL) is one of a pair of cruciate ligaments in the human knee. The two ligaments are also called "cruciform" ligaments, as they are arranged in a crossed formation. In the quadruped stifle joint, based on its anatomical position, it is also referred to as the cranial cruciate ligament. The term cruciate translates to cross. This name is fitting because the ACL crosses the posterior cruciate ligament to form an "X". It is composed of strong, fibrous material and assists in controlling excessive motion. This is done by limiting mobility of the joint. The anterior cruciate ligament is one of the four main ligaments of the knee, providing 85% of the restraining force to anterior tibial displacement at 30 and 90° of knee flexion. The ACL is the most injured ligament of the four located in the knee.

Peroneal nerve paralysis is a paralysis on common fibular nerve that affects patient’s ability to lift the foot at the ankle. The condition was named after Friedrich Albert von Zenker. Peroneal nerve paralysis usually leads to neuromuscular disorder, peroneal nerve injury, or foot drop which can be symptoms of more serious disorders such as nerve compression. The origin of peroneal nerve palsy has been reported to be associated with musculoskeletal injury or isolated nerve traction and compression. Also it has been reported to be mass lesions and metabolic syndromes. Peroneal nerve is most commonly interrupted at the knee and possibly at the joint of hip and ankle. Most studies reported that about 30% of peroneal nerve palsy is followed from knee dislocations.
In medicine, a stinger, also called a burner or nerve pinch injury, is a neurological injury suffered by athletes, mostly in high-contact sports such as ice hockey, rugby, American football, and wrestling. The spine injury is characterized by a shooting or stinging pain that travels down one arm, followed by numbness and weakness in the parts of the arms, including the biceps, deltoid, and spinati muscles. Many athletes in contact sports have suffered stingers, but they are often unreported to medical professionals.

Achilles tendon rupture is when the Achilles tendon, at the back of the ankle, breaks. Symptoms include the sudden onset of sharp pain in the heel. A snapping sound may be heard as the tendon breaks and walking becomes difficult.
The pronator teres is a muscle that, along with the pronator quadratus, serves to pronate the forearm. It has two origins, at the medial humeral supracondylar ridge and the ulnar tuberosity, and inserts near the middle of the radius.

A brachial plexus injury (BPI), also known as brachial plexus lesion, is an injury to the brachial plexus, the network of nerves that conducts signals from the spinal cord to the shoulder, arm and hand. These nerves originate in the fifth, sixth, seventh and eighth cervical (C5–C8), and first thoracic (T1) spinal nerves, and innervate the muscles and skin of the chest, shoulder, arm and hand.

Radial neuropathy is a type of mononeuropathy which results from acute trauma to the radial nerve that extends the length of the arm. It is known as transient paresthesia when sensation is temporarily abnormal.
A selective dorsal rhizotomy (SDR), also known as a rhizotomy, dorsal rhizotomy, or a selective posterior rhizotomy, is a neurosurgical procedure that selectively cut problematic nerve roots of the spinal cord. This procedure has been well-established in the literature as a surgical intervention and is used to relieve negative symptoms of neuromuscular conditions such as spastic diplegia and other forms of spastic cerebral palsy. The specific sensory nerves inducing spasticity are identified using electromyographic (EMG) stimulation and graded on a scale of 1 (mild) to 4. Abnormal nerve responses are isolated and cut, thereby reducing symptoms of spasticity.
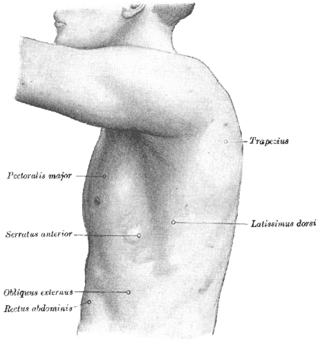
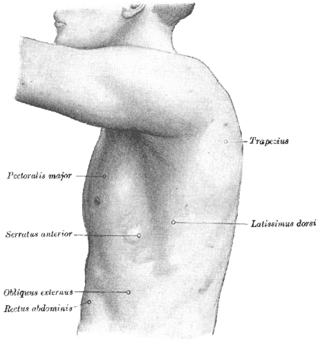
A winged scapula is a skeletal medical condition in which the shoulder blade protrudes from a person's back in an abnormal position.
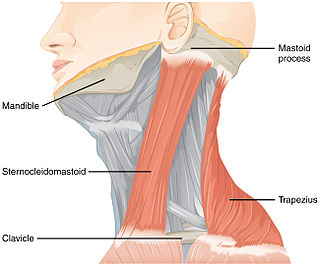
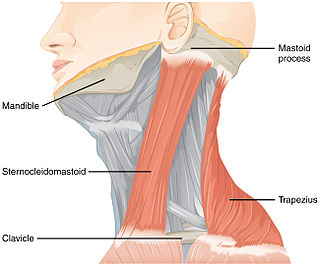
Accessory nerve disorder is an injury to the spinal accessory nerve which results in diminished or absent function of the sternocleidomastoid muscle and upper portion of the trapezius muscle.

Radial tunnel syndrome (RTS) is caused by increased pressure on the radial nerve as it travels from the upper arm to the hand and wrist.

A Holstein–Lewis fracture is a fracture of the distal third of the humerus resulting in entrapment of the radial nerve.

Injuries to the arm, forearm or wrist area can lead to various nerve disorders. One such disorder is median nerve palsy. The median nerve controls the majority of the muscles in the forearm. It controls abduction of the thumb, flexion of hand at wrist, flexion of digital phalanx of the fingers, is the sensory nerve for the first three fingers, etc. Because of this major role of the median nerve, it is also called the eye of the hand. If the median nerve is damaged, the ability to abduct and oppose the thumb may be lost due to paralysis of the thenar muscles. Various other symptoms can occur which may be repaired through surgery and tendon transfers. Tendon transfers have been very successful in restoring motor function and improving functional outcomes in patients with median nerve palsy.

Smile surgery or smile reconstruction is a surgical procedure that restores the smile for people with facial nerve paralysis. Facial nerve paralysis is a relatively common condition with a yearly incidence of 0.25% leading to function loss of the mimic muscles. The facial nerve gives off several branches in the face. If one or more facial nerve branches are paralysed, the corresponding mimetic muscles lose their ability to contract. This may lead to several symptoms such as incomplete eye closure with or without exposure keratitis, oral incompetence, poor articulation, dental caries, drooling, and a low self-esteem. This is because the different branches innervate the frontalis muscle, orbicularis oculi and oris muscles, lip elevators and depressors, and the platysma. The elevators of the upper lip and corner of the mouth are innervated by the zygomatic and buccal branches. When these branches are paralysed, there is an inability to create a symmetric smile.
Upper-limb surgery in tetraplegia includes a number of surgical interventions that can help improve the quality of life of a patient with tetraplegia.

Spastic hemiplegia is a neuromuscular condition of spasticity that results in the muscles on one side of the body being in a constant state of contraction. It is the "one-sided version" of spastic diplegia. It falls under the mobility impairment umbrella of cerebral palsy. About 20–30% of people with cerebral palsy have spastic hemiplegia. Due to brain or nerve damage, the brain is constantly sending action potentials to the neuromuscular junctions on the affected side of the body. Similar to strokes, damage on the left side of the brain affects the right side of the body and damage on the right side of the brain affects the left side of the body. Other side can be effected for lesser extent. The affected side of the body is rigid, weak and has low functional abilities. In most cases, the upper extremity is much more affected than the lower extremity. This could be due to preference of hand usage during early development. If both arms are affected, the condition is referred to as double hemiplegia. Some patients with spastic hemiplegia only experience minor impairments, where in severe cases one side of the body could be completely paralyzed. The severity of spastic hemiplegia is dependent upon the degree of the brain or nerve damage.
The Eden–Lange procedure is an orthopedic procedure to alleviate the symptoms of trapezius palsy when more conservative measures, such as spontaneous resolution and surgical nerve repair are not promising. The rhomboid major, rhomboid minor, and levator scapulae muscles are transferred laterally along the scapula to replace the functions of the lower, middle, and upper fibers of the trapezius, respectively. The transferred muscles hold the scapula in a more medial and upwardly rotated position, without winging.
Nerve glide, also known as nerve flossing or nerve stretching, is an exercise that stretches nerves. It facilitates the smooth and regular movement of peripheral nerves in the body. It allows the nerve to glide freely along with the movement of the joint and relax the nerve from compression. Nerve gliding cannot proceed with injuries or inflammations as the nerve is trapped by the tissue surrounding the nerve near the joint. Thus, nerve gliding exercise is widely used in rehabilitation programs and during the post-surgical period.