Related Research Articles

An anticoagulant, commonly known as a blood thinner, is a chemical substance that prevents or reduces the coagulation of blood, prolonging the clotting time. Some occur naturally in blood-eating animals, such as leeches and mosquitoes, which help keep the bite area unclotted long enough for the animal to obtain blood.
Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets (thrombocytes) and fibrin to form a blood clot to prevent blood loss. Even when a blood vessel is not injured, blood clots may form in the body under certain conditions. A clot, or a piece of the clot, that breaks free and begins to travel around the body is known as an embolus.
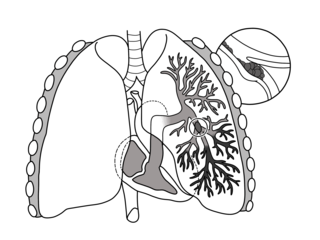
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing in, and coughing up blood. Symptoms of a blood clot in the leg may also be present, such as a red, warm, swollen, and painful leg. Signs of a PE include low blood oxygen levels, rapid breathing, rapid heart rate, and sometimes a mild fever. Severe cases can lead to passing out, abnormally low blood pressure, obstructive shock, and sudden death.

Venous thrombosis is the blockage of a vein caused by a thrombus. A common form of venous thrombosis is deep vein thrombosis (DVT), when a blood clot forms in the deep veins. If a thrombus breaks off (embolizes) and flows to the lungs to lodge there, it becomes a pulmonary embolism (PE), a blood clot in the lungs. The conditions of DVT only, DVT with PE, and PE only, are all captured by the term venous thromboembolism (VTE).
Factor V Leiden is a variant of human factor V, which causes an increase in blood clotting (hypercoagulability). Due to this mutation, protein C, an anticoagulant protein that normally inhibits the pro-clotting activity of factor V, is not able to bind normally to factor V, leading to a hypercoagulable state, i.e., an increased tendency for the patient to form abnormal and potentially harmful blood clots. Factor V Leiden is the most common hereditary hypercoagulability disorder amongst ethnic Europeans. It is named after the Dutch city of Leiden, where it was first identified in 1994 by Rogier Maria Bertina under the direction of Pieter Hendrick Reitsma. Despite the increased risk of venous thromboembolisms, people with one copy of this gene have not been found to have shorter lives than the general population. It is an autosomal dominant genetic disorder with incomplete penetrance.

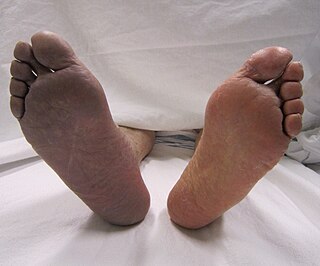
Deep vein thrombosis (DVT) is a type of venous thrombosis involving the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. A minority of DVTs occur in the arms. Symptoms can include pain, swelling, redness, and enlarged veins in the affected area, but some DVTs have no symptoms.
Low-molecular-weight heparin (LMWH) is a class of anticoagulant medications. They are used in the prevention of blood clots and, in the treatment of venous thromboembolism, and the treatment of myocardial infarction.

Thromboembolism is a condition in which a blood clot (thrombus) breaks off from its original site and travels through the bloodstream to obstruct a blood vessel, causing tissue ischemia and organ damage. Thromboembolism can affect both the venous and arterial systems, with different clinical manifestations and management strategies.
D-dimer is a dimer that is a fibrin degradation product, a small protein fragment present in the blood after a blood clot is degraded by fibrinolysis. It is so named because it contains two D fragments of the fibrin protein joined by a cross-link, hence forming a protein dimer.
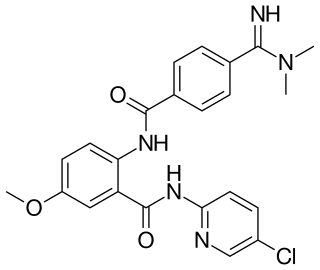
Ximelagatran is an anticoagulant that has been investigated extensively as a replacement for warfarin that would overcome the problematic dietary, drug interaction, and monitoring issues associated with warfarin therapy. In 2006, its manufacturer AstraZeneca announced that it would withdraw pending applications for marketing approval after reports of hepatotoxicity during trials, and discontinue its distribution in countries where the drug had been approved.

Thrombophilia is an abnormality of blood coagulation that increases the risk of thrombosis. Such abnormalities can be identified in 50% of people who have an episode of thrombosis that was not provoked by other causes. A significant proportion of the population has a detectable thrombophilic abnormality, but most of these develop thrombosis only in the presence of an additional risk factor.

Post-thrombotic syndrome (PTS), also called postphlebitic syndrome and venous stress disorder is a medical condition that may occur as a long-term complication of deep vein thrombosis (DVT).
Antithrombin III deficiency is a deficiency of antithrombin III. This deficiency may be inherited or acquired. It is a rare hereditary disorder that generally comes to light when a patient suffers recurrent venous thrombosis and pulmonary embolism, and repetitive intrauterine fetal death (IUFD). Hereditary antithrombin deficiency results in a state of increased coagulation which may lead to venous thrombosis. Inheritance is usually autosomal dominant, though a few recessive cases have been noted. The disorder was first described by Egeberg in 1965. The causes of acquired antithrombin deficiency are easier to find than the hereditary deficiency.

Superficial thrombophlebitis is a thrombosis and inflammation of superficial veins presenting as a painful induration (thickening) with erythema, often in a linear or branching configuration with a cordlike appearance.
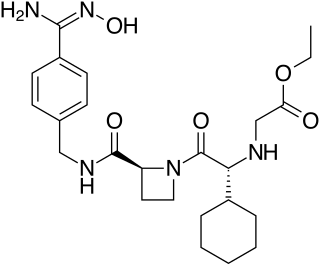
Betrixaban is an oral anticoagulant drug which acts as a direct factor Xa inhibitor. Betrixaban is FDA approved for venous thrombosis prevention in adults hospitalized for an acute illness who are at risk for thromboembolic complications. Compared to other directly acting oral anticoagulants betrixaban has relatively low renal excretion and is not metabolized by CYP3A4.
Prothrombin G20210A is a genetic condition that increases the risk of blood clots including from deep vein thrombosis, and of pulmonary embolism. One copy of the mutation increases the risk of a blood clot from 1 in 1,000 per year to 2.5 in 1,000. Two copies increases the risk to up to 20 in 1,000 per year. Most people never develop a blood clot in their lifetimes.

Thrombosis prevention or thromboprophylaxis is medical treatment to prevent the development of thrombosis in those considered at risk for developing thrombosis. Some people are at a higher risk for the formation of blood clots than others, such as those with cancer undergoing a surgical procedure. Prevention measures or interventions are usually begun after surgery as the associated immobility will increase a person's risk.

Ultrasonography in suspected deep vein thrombosis focuses primarily on the femoral vein and the popliteal vein, because thrombi in these veins are associated with the greatest risk of harmful pulmonary embolism.
Coagulation activation markers are biomarkers of net activation of coagulation and fibrinolysis. Examples include prothrombin fragment 1+2 (F1+2), thrombin–antithrombin complex (TAT), fibrinopeptide A (FpA), fibrin monomers (FMs), plasmin-α2-antiplasmin complex (PAP), activated protein C–protein C inhibitor (APC-PCI), and D-dimer (DD). These compounds are markers of thrombin generation, fibrin generation, and fibrinolysis. Coagulation activation markers, particularly D-dimer, are useful in the diagnosis of acute venous thromboembolism. They may also be useful in the assessment of hypercoagulability and venous thromboembolism risk.

Marie Claire McLintock was a New Zealand haematologist and obstetric physician. She was an expert in medical conditions and disorders related to bleeding and blood clotting, and medical problems associated with pregnancy.
References
- 1 2 Antic, Darko; Milic, Natasa; Nikolovski, Srdjan; Todorovic, Milena; Bila, Jelena; Djurdjevic, Predrag; Andjelic, Bosko; Djurasinovic, Vladislava; Sretenovic, Aleksandra; Vukovic, Vojin; Jelicic, Jelena (October 2016). "Development and validation of multivariable predictive model for thromboembolic events in lymphoma patients: Multivariable Predictive Model". American Journal of Hematology. 91 (10): 1014–1019. doi: 10.1002/ajh.24466 . PMID 27380861. S2CID 1724916.
- 1 2 Abdel-Razeq, Hikmat; Ma’koseh, Mohammad; Mansour, Asem; Bater, Rayan; Amarin, Rula; Abufara, Alaa; Halahleh, Khalid; Manassra, Mohammad; Alrwashdeh, Mohammad; Almomani, Mohammad; Zmaily, Mais (January 2021). "The Application of the ThroLy Risk Assessment Model to Predict Venous Thromboembolism in Patients with Diffuse Large B-Cell Lymphoma". Clinical and Applied Thrombosis/Hemostasis. 27: 107602962110459. doi:10.1177/10760296211045908. ISSN 1076-0296. PMC 8642105 . PMID 34590497.
- ↑ Ma’koseh, Mohammad; Abufara, Alaa; Albaghdadi, Dana; Ghalayni, Ruba; Abdel-Razeq, Sarah; Alzughali, Eman; Abdel Rahman, Fadwa; Alhalaseh, Yazan; Halahleh, Khalid; Abdel-Razeq, Hikmat (2024-01-12). "The Application of Existing Risk Assessment Models (RAMS) to Predict the Occurrence of Venous Thromboembolic Events among Patients with Classic Hodgkin Lymphoma". Journal of Clinical Medicine. 13 (2): 436. doi: 10.3390/jcm13020436 . ISSN 2077-0383. PMC 10816014 . PMID 38256570.
- ↑ Sánchez Prieto, Irene; Gutiérrez Jomarrón, Isabel; Martínez Vázquez, Celia; Rodríguez Barquero, Pedro; Gili Herreros, Paula; García-Suárez, Julio (2024-04-27). "Comprehensive evaluation of genetic and acquired thrombophilia markers for an individualized prediction of clinical thrombosis in patients with lymphoma and multiple myeloma". Journal of Thrombosis and Thrombolysis. doi: 10.1007/s11239-024-02977-0 . ISSN 1573-742X.
- ↑ Leviatan, Ilona; Ellis, Martin H. (December 2023). "Use of direct oral anticoagulants in hematologic malignancies". Thrombosis Update. 13: 100152. doi: 10.1016/j.tru.2023.100152 .
- ↑ Rupa-Matysek, Joanna; Brzeźniakiewicz-Janus, Katarzyna; Gil, Lidia; Krasiński, Zbigniew; Komarnicki, Mieczysław (July 2018). "Evaluation of the ThroLy score for the prediction of venous thromboembolism in newly diagnosed patients treated for lymphoid malignancies in clinical practice". Cancer Medicine. 7 (7): 2868–2875. doi:10.1002/cam4.1540. PMC 6051175 . PMID 29761831.
- ↑ Antic, Darko; Milic, Natasa; Mihaljevic, Biljana; Cheson, Bruce; Narkhede, Mayur; Abdel-Razeq, Hikmat; Panovska, Irina; Trajkova, Sanja; Popova, Marija; Aurer, Igor; Boban, Ana (November 29, 2018). "External Validation and Revision of Thrombosis Lymphoma /Throly/ Score". Blood. 132 (Supplement 1): 140. doi: 10.1182/blood-2018-99-115568 . ISSN 0006-4971.
- ↑ Assanto, Giovanni Manfredi; Salvatori, Martina; Pontecorvo, Sara; Maiorana, Gianluca; Cenfra, Natalia; D’elia, Gianna Maria; Bianchi, Maria Paola; Annechini, Giorgia; Santoro, Cristina Santoro; Martelli, Maurizio; Tafuri, Agostino; Pulsoni, Alessandro; Del Giudice, Ilaria; Chistolini, Antonio (August 2023). "S219: Predicting Thrombotic Risk in Patients with Hodgkin Lymphoma: A Multicentric Study of Throly and Khorana Risk Scores". HemaSphere. 7 (S3): e700140a. doi:10.1097/01.HS9.0000967788.70014.0a. ISSN 2572-9241. PMC 10428474 .