Thrombosis is the formation of a blood clot inside a blood vessel, obstructing the flow of blood through the circulatory system. When a blood vessel is injured, the body uses platelets (thrombocytes) and fibrin to form a blood clot to prevent blood loss. Even when a blood vessel is not injured, blood clots may form in the body under certain conditions. A clot, or a piece of the clot, that breaks free and begins to travel around the body is known as an embolus.
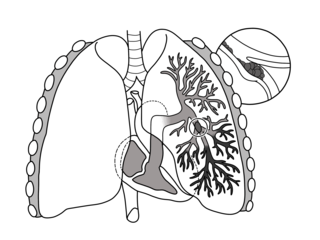
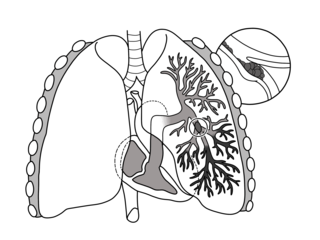
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing in, and coughing up blood. Symptoms of a blood clot in the leg may also be present, such as a red, warm, swollen, and painful leg. Signs of a PE include low blood oxygen levels, rapid breathing, rapid heart rate, and sometimes a mild fever. Severe cases can lead to passing out, abnormally low blood pressure, obstructive shock, and sudden death.

Venous thrombosis is the blockage of a vein caused by a thrombus. A common form of venous thrombosis is deep vein thrombosis (DVT), when a blood clot forms in the deep veins. If a thrombus breaks off (embolizes) and flows to the lungs to lodge there, it becomes a pulmonary embolism (PE), a blood clot in the lungs. The conditions of DVT only, DVT with PE, and PE only, are all captured by the term venous thromboembolism (VTE).

Antiphospholipid syndrome, or antiphospholipid antibody syndrome, is an autoimmune, hypercoagulable state caused by antiphospholipid antibodies. APS can lead to blood clots (thrombosis) in both arteries and veins, pregnancy-related complications, and other symptoms like low platelets, kidney disease, heart disease, and rash. Although the exact etiology of APS is still not clear, genetics is believed to play a key role in the development of the disease.
Factor V Leiden is a variant of human factor V, which causes an increase in blood clotting (hypercoagulability). Due to this mutation, protein C, an anticoagulant protein that normally inhibits the pro-clotting activity of factor V, is not able to bind normally to factor V, leading to a hypercoagulable state, i.e., an increased tendency for the patient to form abnormal and potentially harmful blood clots. Factor V Leiden is the most common hereditary hypercoagulability disorder amongst ethnic Europeans. It is named after the Dutch city of Leiden, where it was first identified in 1994 by Rogier Maria Bertina under the direction of Pieter Hendrick Reitsma. Despite the increased risk of venous thromboembolisms, people with one copy of this gene have not been found to have shorter lives than the general population. It is an autosomal dominant genetic disorder with incomplete penetrance.

Deep vein thrombosis (DVT) is a type of venous thrombosis involving the formation of a blood clot in a deep vein, most commonly in the legs or pelvis. A minority of DVTs occur in the arms. Symptoms can include pain, swelling, redness, and enlarged veins in the affected area, but some DVTs have no symptoms.

Vascular surgery is a surgical subspecialty in which vascular diseases involving the arteries, veins, or lymphatic vessels, are managed by medical therapy, minimally-invasive catheter procedures and surgical reconstruction. The specialty evolved from general and cardiovascular surgery where it refined the management of just the vessels, no longer treating the heart or other organs. Modern vascular surgery includes open surgery techniques, endovascular techniques and medical management of vascular diseases - unlike the parent specialities. The vascular surgeon is trained in the diagnosis and management of diseases affecting all parts of the vascular system excluding the coronaries and intracranial vasculature. Vascular surgeons also are called to assist other physicians to carry out surgery near vessels, or to salvage vascular injuries that include hemorrhage control, dissection, occlusion or simply for safe exposure of vascular structures.

Thromboembolism is a condition in which a blood clot (thrombus) breaks off from its original site and travels through the bloodstream to obstruct a blood vessel, causing tissue ischemia and organ damage. Thromboembolism can affect both the venous and arterial systems, with different clinical manifestations and management strategies.

Thrombophilia is an abnormality of blood coagulation that increases the risk of thrombosis. Such abnormalities can be identified in 50% of people who have an episode of thrombosis that was not provoked by other causes. A significant proportion of the population has a detectable thrombophilic abnormality, but most of these develop thrombosis only in the presence of an additional risk factor.

Renal vein thrombosis (RVT) is the formation of a clot in the vein that drains blood from the kidneys, ultimately leading to a reduction in the drainage of one or both kidneys and the possible migration of the clot to other parts of the body. First described by German pathologist Friedrich Daniel von Recklinghausen in 1861, RVT most commonly affects two subpopulations: newly born infants with blood clotting abnormalities or dehydration and adults with nephrotic syndrome.

May–Thurner syndrome (MTS), also known as the iliac vein compression syndrome, is a condition in which compression of the common venous outflow tract of the left lower extremity may cause discomfort, swelling, pain or iliofemoral deep vein thrombosis.
Catastrophic antiphospholipid syndrome (CAPS), also known as Asherson's syndrome, is a rare autoimmune disease in which widespread, intravascular clotting causes multi-organ failure. The syndrome is caused by antiphospholipid antibodies that target a group of proteins in the body that are associated with phospholipids. These antibodies activate endothelial cells, platelets, and immune cells, ultimately causing a large inflammatory immune response and widespread clotting. CAPS was first described by Ronald Asherson in 1992. The syndrome exhibits thrombotic microangiopathy, multiple organ thromboses, and in some cases tissue necrosis and is considered an extreme or catastrophic variant of the antiphospholipid syndrome.

Vascular disease is a class of diseases of the vessels of the circulatory system in the body, including blood vessels – the arteries and veins, and the lymphatic vessels. Vascular disease is a subgroup of cardiovascular disease. Disorders in this vast network of blood and lymph vessels can cause a range of health problems that can sometimes become severe, and fatal. Coronary heart disease for example, is the leading cause of death for men and women in the United States.

Post-thrombotic syndrome (PTS), also called postphlebitic syndrome and venous stress disorder is a medical condition that may occur as a long-term complication of deep vein thrombosis (DVT).
Hypercoagulability in pregnancy is the propensity of pregnant women to develop thrombosis. Pregnancy itself is a factor of hypercoagulability, as a physiologically adaptive mechanism to prevent post partum bleeding. However, when combined with an additional underlying hypercoagulable states, the risk of thrombosis or embolism may become substantial.
Embolectomy is the emergency interventional or surgical removal of emboli which are blocking blood circulation. It usually involves removal of thrombi, and is then referred to as thromboembolectomy or thrombectomy. Embolectomy is an emergency procedure often as the last resort because permanent occlusion of a significant blood flow to an organ leads to necrosis. Other involved therapeutic options are anticoagulation and thrombolysis.

Superficial thrombophlebitis is a thrombosis and inflammation of superficial veins presenting as a painful induration (thickening) with erythema, often in a linear or branching configuration with a cordlike appearance.
Prothrombin G20210A is a genetic condition that increases the risk of blood clots including from deep vein thrombosis, and of pulmonary embolism. One copy of the mutation increases the risk of a blood clot from 1 in 1,000 per year to 2.5 in 1,000. Two copies increases the risk to up to 20 in 1,000 per year. Most people never develop a blood clot in their lifetimes.

Superficial vein thrombosis (SVT) is a blood clot formed in a superficial vein, a vein near the surface of the body. Usually there is thrombophlebitis, which is an inflammatory reaction around a thrombosed vein, presenting as a painful induration with redness. SVT itself has limited significance when compared to a deep vein thrombosis (DVT), which occurs deeper in the body at the deep venous system level. However, SVT can lead to serious complications, and is therefore no longer regarded as a benign condition. If the blood clot is too near the saphenofemoral junction there is a higher risk of pulmonary embolism, a potentially life-threatening complication.

Thrombosis prevention or thromboprophylaxis is medical treatment to prevent the development of thrombosis in those considered at risk for developing thrombosis. Some people are at a higher risk for the formation of blood clots than others, such as those with cancer undergoing a surgical procedure. Prevention measures or interventions are usually begun after surgery as the associated immobility will increase a person's risk.