Hepatitis is inflammation of the liver tissue. Some people or animals with hepatitis have no symptoms, whereas others develop yellow discoloration of the skin and whites of the eyes (jaundice), poor appetite, vomiting, tiredness, abdominal pain, and diarrhea. Hepatitis is acute if it resolves within six months, and chronic if it lasts longer than six months. Acute hepatitis can resolve on its own, progress to chronic hepatitis, or (rarely) result in acute liver failure. Chronic hepatitis may progress to scarring of the liver (cirrhosis), liver failure, and liver cancer.

Jaundice, also known as icterus, is a yellowish or greenish pigmentation of the skin and sclera due to high bilirubin levels. Jaundice in adults is typically a sign indicating the presence of underlying diseases involving abnormal heme metabolism, liver dysfunction, or biliary-tract obstruction. The prevalence of jaundice in adults is rare, while jaundice in babies is common, with an estimated 80% affected during their first week of life. The most commonly associated symptoms of jaundice are itchiness, pale feces, and dark urine.

Bilirubin (BR) is a red-orange compound that occurs in the normal catabolic pathway that breaks down heme in vertebrates. This catabolism is a necessary process in the body's clearance of waste products that arise from the destruction of aged or abnormal red blood cells. In the first step of bilirubin synthesis, the heme molecule is stripped from the hemoglobin molecule. Heme then passes through various processes of porphyrin catabolism, which varies according to the region of the body in which the breakdown occurs. For example, the molecules excreted in the urine differ from those in the feces. The production of biliverdin from heme is the first major step in the catabolic pathway, after which the enzyme biliverdin reductase performs the second step, producing bilirubin from biliverdin.
Liver function tests, also referred to as a hepatic panel or liver panel, are groups of blood tests that provide information about the state of a patient's liver. These tests include prothrombin time (PT/INR), activated partial thromboplastin time (aPTT), albumin, bilirubin, and others. The liver transaminases aspartate transaminase and alanine transaminase are useful biomarkers of liver injury in a patient with some degree of intact liver function.

Alcoholic liver disease (ALD), also called alcohol-related liver disease (ARLD), is a term that encompasses the liver manifestations of alcohol overconsumption, including fatty liver, alcoholic hepatitis, and chronic hepatitis with liver fibrosis or cirrhosis.

Gilbert syndrome (GS) is a syndrome in which the liver of affected individuals processes bilirubin more slowly than the majority. Many people never have symptoms. Occasionally jaundice may occur.

Hemolytic anemia or haemolytic anaemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells (RBCs), either in the blood vessels or elsewhere in the human body (extravascular). This most commonly occurs within the spleen, but also can occur in the reticuloendothelial system or mechanically. Hemolytic anemia accounts for 5% of all existing anemias. It has numerous possible consequences, ranging from general symptoms to life-threatening systemic effects. The general classification of hemolytic anemia is either intrinsic or extrinsic. Treatment depends on the type and cause of the hemolytic anemia.

Alcoholic hepatitis is hepatitis due to excessive intake of alcohol. Patients typically have a history of at least 10 years of heavy alcohol intake, typically 8–10 drinks per day. It is usually found in association with fatty liver, an early stage of alcoholic liver disease, and may contribute to the progression of fibrosis, leading to cirrhosis. Symptoms may present acutely after a large amount of alcoholic intake in a short time period, or after years of excess alcohol intake. Signs and symptoms of alcoholic hepatitis include jaundice, ascites, fatigue and hepatic encephalopathy. Mild cases are self-limiting, but severe cases have a high risk of death. Severity in alcoholic hepatitis is determined several clinical prediction models such as the Maddrey's Discriminant Function and the MELD score.

Liver disease, or hepatic disease, is any of many diseases of the liver. If long-lasting it is termed chronic liver disease. Although the diseases differ in detail, liver diseases often have features in common.
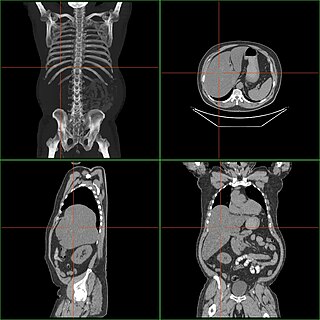
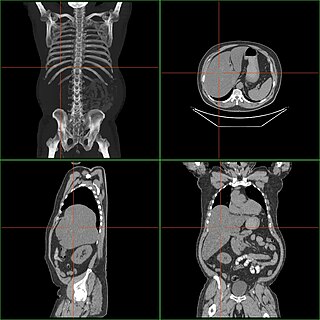
Hepatomegaly is enlargement of the liver. It is a non-specific medical sign, having many causes, which can broadly be broken down into infection, hepatic tumours, and metabolic disorder. Often, hepatomegaly presents as an abdominal mass. Depending on the cause, it may sometimes present along with jaundice.

Acanthocyte, in biology and medicine, refers to an abnormal form of red blood cell that has a spiked cell membrane, due to thorny projections. A similar term is spur cells. Often they may be confused with echinocytes or schistocytes.

Neonatal jaundice is a yellowish discoloration of the white part of the eyes and skin in a newborn baby due to high bilirubin levels. Other symptoms may include excess sleepiness or poor feeding. Complications may include seizures, cerebral palsy, or kernicterus.
Chronic liver disease in the clinical context is a disease process of the liver that involves a process of progressive destruction and regeneration of the liver parenchyma leading to fibrosis and cirrhosis. "Chronic liver disease" refers to disease of the liver which lasts over a period of six months. It consists of a wide range of liver pathologies which include inflammation, liver cirrhosis, and hepatocellular carcinoma. The entire spectrum need not be experienced.

Crigler–Najjar syndrome is a rare inherited disorder affecting the metabolism of bilirubin, a chemical formed from the breakdown of the heme in red blood cells. The disorder results in a form of nonhemolytic jaundice, which results in high levels of unconjugated bilirubin and often leads to brain damage in infants. The disorder is inherited in an autosomal recessive manner. The annual incidence is estimated at 1 in 1,000,000.

Steatohepatitis is a type of fatty liver disease, characterized by inflammation of the liver with concurrent fat accumulation in liver. Mere deposition of fat in the liver is termed steatosis, and together these constitute fatty liver changes.

Hereditary hyperbilirubinemia refers to a group of conditions where levels of bilirubin, a byproduct of red blood cell metabolism, are elevated in the blood due to a genetic cause. Various mutations of enzymes in the liver cells, which breakdown bilirubin, cause varying elevated levels of bilirubin in the blood. These disorders may cause yellowing of the skin and eyes, called jaundice.

Cirrhosis, also known as liver cirrhosis or hepatic cirrhosis, chronic liver failure or chronic hepatic failure and end-stage liver disease, is a condition of the liver in which the normal functioning tissue, or parenchyma, is replaced with scar tissue (fibrosis) and regenerative nodules as a result of chronic liver disease. Damage to the liver leads to repair of liver tissue and subsequent formation of scar tissue. Over time, scar tissue and nodules of regenerating hepatocytes can replace the parenchyma, causing increased resistance to blood flow in the liver's capillaries—the hepatic sinusoids—and consequently portal hypertension, as well as impairment in other aspects of liver function. The disease typically develops slowly over months or years.

Bilirubin glucuronide is a water-soluble reaction intermediate over the process of conjugation of indirect bilirubin. Bilirubin glucuronide itself belongs to the category of conjugated bilirubin along with bilirubin di-glucuronide. However, only the latter one is primarily excreted into the bile in the normal setting.
Hemolytic jaundice, also known as prehepatic jaundice, is a type of jaundice arising from hemolysis or excessive destruction of red blood cells, when the byproduct bilirubin is not excreted by the hepatic cells quickly enough. Unless the patient is concurrently affected by hepatic dysfunctions or is experiencing hepatocellular damage, the liver does not contribute to this type of jaundice.
Hyperbilirubinemia is a clinical condition describing an elevation of blood bilirubin level due to the inability to properly metabolise or excrete bilirubin, a product of erythrocytes breakdown. In severe cases, it is manifested as jaundice, the yellowing of tissues like skin and the sclera when excess bilirubin deposits in them. The US records 52,500 jaundice patients annually. By definition, bilirubin concentration of greater than 3 mg/dL is considered hyperbilirubinemia, following which jaundice progressively develops and becomes apparent when plasma levels reach 20 mg/dL. Rather than a disease itself, hyperbilirubinemia is indicative of multifactorial underlying disorders that trace back to deviations from regular bilirubin metabolism. Diagnosis of hyperbilirubinemia depends on physical examination, urinalysis, serum tests, medical history and imaging to identify the cause. Genetic diseases, alcohol, pregnancy and hepatitis viruses affect the likelihood of hyperbilirubinemia. Causes of hyperbilirubinemia mainly arise from the liver. These include haemolytic anaemias, enzymatic disorders, liver damage and gallstones. Hyperbilirubinemia itself is often benign. Only in extreme cases does kernicterus, a type of brain injury, occur. Therapy for adult hyperbilirubinemia targets the underlying diseases but patients with jaundice often have poor outcomes.