Tetralogy of Fallot (TOF), formerly known as Steno-Fallot tetralogy, is a congenital heart defect characterized by four specific cardiac defects. Classically, the four defects are:

Atrial septal defect (ASD) is a congenital heart defect in which blood flows between the atria of the heart. Some flow is a normal condition both pre-birth and immediately post-birth via the foramen ovale; however, when this does not naturally close after birth it is referred to as a patent (open) foramen ovale (PFO). It is common in patients with a congenital atrial septal aneurysm (ASA).

A congenital heart defect (CHD), also known as a congenital heart anomaly and congenital heart disease, is a defect in the structure of the heart or great vessels that is present at birth. A congenital heart defect is classed as a cardiovascular disease. Signs and symptoms depend on the specific type of defect. Symptoms can vary from none to life-threatening. When present, symptoms may include rapid breathing, bluish skin (cyanosis), poor weight gain, and feeling tired. CHD does not cause chest pain. Most congenital heart defects are not associated with other diseases. A complication of CHD is heart failure.

An acyanotic heart defect, is a class of congenital heart defects. In these, blood is shunted (flows) from the left side of the heart to the right side of the heart, most often due to a structural defect (hole) in the interventricular septum. People often retain normal levels of oxyhemoglobin saturation in systemic circulation.
A cyanotic heart defect is any congenital heart defect (CHD) that occurs due to deoxygenated blood bypassing the lungs and entering the systemic circulation, or a mixture of oxygenated and unoxygenated blood entering the systemic circulation. It is caused by structural defects of the heart such as right-to-left or bidirectional shunting, malposition of the great arteries, or any condition which increases pulmonary vascular resistance. The result may be the development of collateral circulation.
The Rastelli procedure is an open heart surgical procedure developed by Italian physician and cardiac surgery researcher, Giancarlo Rastelli, in 1967 at the Mayo Clinic, and involves using a pulmonary or aortic homograft conduit to relieve pulmonary obstruction in double outlet right ventricle with pulmonary stenosis.
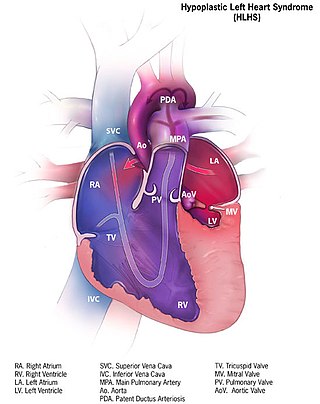
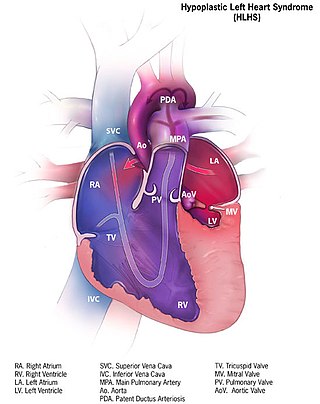
Hypoplastic left heart syndrome (HLHS) is a rare congenital heart defect in which the left side of the heart is severely underdeveloped and incapable of supporting the systemic circulation. It is estimated to account for 2-3% of all congenital heart disease. Early signs and symptoms include poor feeding, cyanosis, and diminished pulse in the extremities. The etiology is believed to be multifactorial resulting from a combination of genetic mutations and defects resulting in altered blood flow in the heart.

Transposition of the great vessels (TGV) is a group of congenital heart defects involving an abnormal spatial arrangement of any of the great vessels: superior and/or inferior venae cavae, pulmonary artery, pulmonary veins, and aorta. Congenital heart diseases involving only the primary arteries belong to a sub-group called transposition of the great arteries (TGA), which is considered the most common congenital heart lesion that presents in neonates.

Tricuspid atresia is a form of congenital heart disease whereby there is a complete absence of the tricuspid valve. Therefore, there is an absence of right atrioventricular connection. This leads to a hypoplastic (undersized) or absent right ventricle. This defect is contracted during prenatal development, when the heart does not finish developing. It causes the systemic circulation to be filled with relatively deoxygenated blood. The causes of tricuspid atresia are unknown.

The fossa ovalis is a depression in the right atrium of the heart, at the level of the interatrial septum, the wall between right and left atrium. The fossa ovalis is the remnant of a thin fibrous sheet that covered the foramen ovale during fetal development.
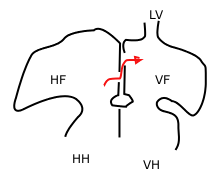
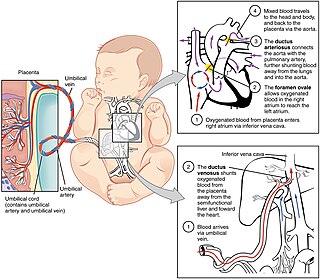
In the fetal heart, the foramen ovale, also foramen Botalli, or the ostium secundum of Born, allows blood to enter the left atrium from the right atrium. It is one of two fetal cardiac shunts, the other being the ductus arteriosus. Another similar adaptation in the fetus is the ductus venosus. In most individuals, the foramen ovale closes at birth. It later forms the fossa ovalis.
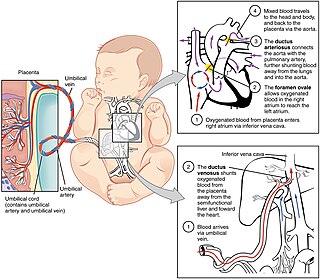
In humans, the circulatory system is different before and after birth. The fetal circulation is composed of the placenta, umbilical blood vessels encapsulated by the umbilical cord, heart and systemic blood vessels. A major difference between the fetal circulation and postnatal circulation is that the lungs are not used during the fetal stage resulting in the presence of shunts to move oxygenated blood and nutrients from the placenta to the fetal tissue. At birth, the start of breathing and the severance of the umbilical cord prompt various changes that quickly transform fetal circulation into postnatal circulation.
Levo-Transposition of the great arteries is an acyanotic congenital heart defect in which the primary arteries are transposed, with the aorta anterior and to the left of the pulmonary artery; the morphological left and right ventricles with their corresponding atrioventricular valves are also transposed.
Pulmonic stenosis, is a dynamic or fixed obstruction of flow from the right ventricle of the heart to the pulmonary artery. It is usually first diagnosed in childhood.

Arterial switch operation (ASO) or arterial switch, is an open heart surgical procedure used to correct dextro-transposition of the great arteries (d-TGA).
A cardiac shunt is a pattern of blood flow in the heart that deviates from the normal circuit of the circulatory system. It may be described as right-left, left-right or bidirectional, or as systemic-to-pulmonary or pulmonary-to-systemic. The direction may be controlled by left and/or right heart pressure, a biological or artificial heart valve or both. The presence of a shunt may also affect left and/or right heart pressure either beneficially or detrimentally.

Atrial septostomy is a surgical procedure in which a small hole is created between the upper two chambers of the heart, the atria. This procedure is primarily used to palliate dextro-Transposition of the great arteries or d-TGA, a life-threatening cyanotic congenital heart defect seen in infants. It is performed prior to an arterial switch operation. Atrial septostomy has also seen limited use as a surgical treatment for pulmonary hypertension. The first atrial septostomy was developed by Vivien Thomas in a canine model and performed in humans by Alfred Blalock. The Rashkind balloon procedure, a common atrial septostomy technique, was developed in 1966 by American cardiologist William Rashkind at the Children's Hospital of Philadelphia.
Hypoplastic right heart syndrome is a congenital heart defect in which the right atrium and right ventricle are underdeveloped. This defect causes inadequate blood flow to the lungs and thus, a blue or cyanotic infant.
The Senning procedure is an atrial switch heart operation performed to treat transposition of the great arteries. It is named after its inventor, the Swedish cardiac surgeon Åke Senning (1915–2000), also known for implanting the first permanent cardiac pacemaker in 1958.