An antiplatelet drug (antiaggregant), also known as a platelet agglutination inhibitor or platelet aggregation inhibitor, is a member of a class of pharmaceuticals that decrease platelet aggregation and inhibit thrombus formation. They are effective in the arterial circulation where classical Vitamin K antagonist anticoagulants have minimal effect.

Platelets or thrombocytes are a component of blood whose function is to react to bleeding from blood vessel injury by clumping, thereby initiating a blood clot. Platelets have no cell nucleus; they are fragments of cytoplasm derived from the megakaryocytes of the bone marrow or lung, which then enter the circulation. Platelets are found only in mammals, whereas in other vertebrates, thrombocytes circulate as intact mononuclear cells.

Coagulation, also known as clotting, is the process by which blood changes from a liquid to a gel, forming a blood clot. It results in hemostasis, the cessation of blood loss from a damaged vessel, followed by repair. The process of coagulation involves activation, adhesion and aggregation of platelets, as well as deposition and maturation of fibrin.

Fibrinogen is a glycoprotein complex, produced in the liver, that circulates in the blood of all vertebrates. During tissue and vascular injury, it is converted enzymatically by thrombin to fibrin and then to a fibrin-based blood clot. Fibrin clots function primarily to occlude blood vessels to stop bleeding. Fibrin also binds and reduces the activity of thrombin. This activity, sometimes referred to as antithrombin I, limits clotting. Fibrin also mediates blood platelet and endothelial cell spreading, tissue fibroblast proliferation, capillary tube formation, and angiogenesis and thereby promotes revascularization and wound healing.

Von Willebrand disease (VWD) is the most common hereditary blood-clotting disorder in humans. An acquired form can sometimes result from other medical conditions. It arises from a deficiency in the quality or quantity of von Willebrand factor (VWF), a multimeric protein that is required for platelet adhesion. It is known to affect several breeds of dogs as well as humans. The three forms of VWD are hereditary, acquired, and pseudo or platelet type. The three types of hereditary VWD are VWD type 1, VWD type 2, and VWD type 3. Type 2 contains various subtypes. Platelet type VWD is also an inherited condition.

Abciximab, a glycoprotein IIb/IIIa receptor antagonist manufactured by Janssen Biologics BV and distributed by Eli Lilly under the trade name ReoPro, is a platelet aggregation inhibitor mainly used during and after coronary artery procedures like angioplasty to prevent platelets from sticking together and causing thrombus formation within the coronary artery. It is a glycoprotein IIb/IIIa inhibitor.
Leukocyte adhesion deficiency (LAD) is a rare autosomal recessive disorder characterized by immunodeficiency resulting in recurrent infections. LAD is currently divided into three subtypes: LAD1, LAD2, and the recently described LAD3, also known as LAD-1/variant. In LAD3, the immune defects are supplemented by a Glanzmann thrombasthenia-like bleeding tendency.

Bernard–Soulier syndrome (BSS) is a rare autosomal recessive bleeding disorder that is caused by a deficiency of the glycoprotein Ib-IX-V complex (GPIb-IX-V), the receptor for von Willebrand factor. The incidence of BSS is estimated to be less than 1 case per million persons, based on cases reported from Europe, North America, and Japan. BSS is a giant platelet disorder, meaning that it is characterized by abnormally large platelets.
In medicine, glycoprotein IIb/IIIa inhibitors, also GpIIb/IIIa inhibitors, is a class of antiplatelet agents.
In biochemistry and medicine, glycoprotein IIb/IIIa is an integrin complex found on platelets. It is a transmembrane receptor for fibrinogen and von Willebrand factor, and aids platelet activation. The complex is formed via calcium-dependent association of gpIIb and gpIIIa, a required step in normal platelet aggregation and endothelial adherence. Platelet activation by ADP leads to the aforementioned conformational change in platelet gpIIb/IIIa receptors that induces binding to fibrinogen. The gpIIb/IIIa receptor is a target of several drugs including abciximab, eptifibatide, and tirofiban.

Tirofiban, sold under the brand name Aggrastat, is an antiplatelet medication. It belongs to a class of antiplatelets named glycoprotein IIb/IIIa inhibitors. Tirofiban is a small molecule inhibitor of the protein-protein interaction between fibrinogen and the platelet integrin receptor GP IIb/IIIa and is the first drug candidate whose origins can be traced to a pharmacophore-based virtual screening lead.

Ristocetin is a glycopeptide antibiotic, obtained from Amycolatopsis lurida, previously used to treat staphylococcal infections. It is no longer used clinically because it caused thrombocytopenia and platelet agglutination. It is now used solely to assay those functions in vitro in the diagnosis of conditions such as von Willebrand disease (vWD) and Bernard–Soulier syndrome. Platelet agglutination caused by ristocetin can occur only in the presence of von Willebrand factor multimers, so if ristocetin is added to blood lacking the factor, the platelets will not clump.

Bivalirudin, sold under the brand names Angiomax and Angiox, among others, is a specific and reversible direct thrombin inhibitor (DTI). Chemically, it is a synthetic congener of the naturally occurring drug hirudin, found in the saliva of the medicinal leech Hirudo medicinalis. It is manufactured by The Medicines Company.

Integrin beta-3 (β3) or CD61 is a protein that in humans is encoded by the ITGB3 gene. CD61 is a cluster of differentiation found on thrombocytes.
The dysfibrinogenemias consist of three types of fibrinogen disorders in which a critical blood clotting factor, fibrinogen, circulates at normal levels but is dysfunctional. Congenital dysfibrinogenemia is an inherited disorder in which one of the parental genes produces an abnormal fibrinogen. This fibrinogen interferes with normal blood clotting and/or lysis of blood clots. The condition therefore may cause pathological bleeding and/or thrombosis. Acquired dysfibrinogenemia is a non-hereditary disorder in which fibrinogen is dysfunctional due to the presence of liver disease, autoimmune disease, a plasma cell dyscrasias, or certain cancers. It is associated primarily with pathological bleeding. Hereditary fibrinogen Aα-Chain amyloidosis is a sub-category of congenital dysfibrinogenemia in which the dysfunctional fibrinogen does not cause bleeding or thrombosis but rather gradually accumulates in, and disrupts the function of, the kidney.

Integrin alpha-IIb is a protein that in humans is encoded by the ITGA2B gene. ITGA2B, also known as CD41, encodes integrin alpha chain 2b. Integrins are heterodimeric integral membrane proteins composed of an alpha chain and a beta chain. Alpha chain 2b undergoes post-translational cleavage to yield disulfide-linked light and heavy chains that join with beta 3 to form a fibrinogen receptor expressed in platelets that plays a crucial role in coagulation. Mutations that interfere with this role result in thrombasthenia. At least 38 disease-causing mutations in this gene have been discovered. In addition to adhesion, integrins are known to participate in cell-surface mediated signalling.
Platelet membrane glycoproteins are surface glycoproteins found on platelets (thrombocytes) which play a key role in hemostasis. When the blood vessel wall is damaged, platelet membrane glycoproteins interact with the extracellular matrix.
The ristocetin-induced platelet aggregation (RIPA) is an ex vivo assay for live platelet function. It measures platelet aggregation with the help of von Willebrand factor (vWF) and exogenous antibiotic ristocetin added in a graded fashion. It is similar to the ristocetin cofactor assay but has the added benefit in that it helps in the diagnosis of type 2B/pseudo von Willebrand disease (vWD) and Bernard–Soulier syndrome because it uses patient's live endogenous platelets, whereas ristocetin cofactor assay tests the function of only the vWF and not the platelets. Ristocetin cofactor assay uses the patient's platelet poor plasma and adds ristocetin and exogenous formalin-fixed platelets which can passively agglutinate. Formalin does not allow the extrinsic platelets to secrete the vWF of their α-granules, and thus only the activity of the intrinsic vWF is tested.
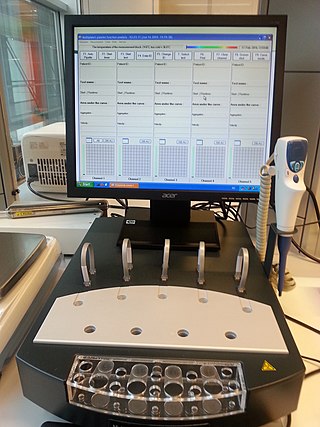
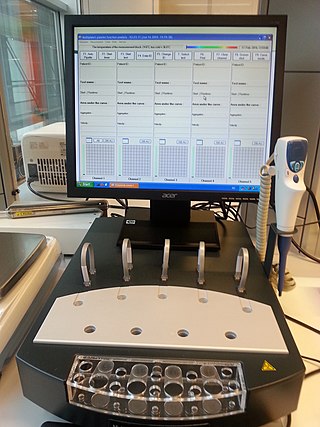
Multiplate multiple electrode aggregometry (MEA) is a test of platelet function in whole blood. The test can be used to diagnose platelet disorders, monitor antiplatelet therapy, and is also investigated as a potential predictor of transfusion requirements and bleeding risk in cardiac surgery.
The platelet plug, also known as the hemostatic plug or platelet thrombus, is an aggregation of platelets formed during early stages of hemostasis in response to one or more injuries to blood vessel walls. After platelets are recruited and begin to accumulate around the breakage, their “sticky” nature allows them to adhere to each other. This forms a platelet plug, which prevents more blood from leaving the body as well as any outside contaminants from getting in. The plug provides a temporary blockage of the break in the vasculature. As such, platelet plug formation occurs after vasoconstriction of the blood vessels but before the creation of the fibrin mesh clot, which is the more permanent solution to the injury. The result of the platelet plug formation is the coagulation of blood. It can also be referred to as primary hemostasis.