Related Research Articles

Antiviral drugs are a class of medication used for treating viral infections. Most antivirals target specific viruses, while a broad-spectrum antiviral is effective against a wide range of viruses. Antiviral drugs are a class of antimicrobials, a larger group which also includes antibiotic, antifungal and antiparasitic drugs, or antiviral drugs based on monoclonal antibodies. Most antivirals are considered relatively harmless to the host, and therefore can be used to treat infections. They should be distinguished from virucides, which are not medication but deactivate or destroy virus particles, either inside or outside the body. Natural virucides are produced by some plants such as eucalyptus and Australian tea trees.
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs as a strategy to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle. The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same-sex and opposite-sex partners so long as the HIV-positive partner maintains an undetectable viral load.

Stavudine (d4T), sold under the brand name Zerit among others, is an antiretroviral medication used to prevent and treat HIV/AIDS. It is generally recommended for use with other antiretrovirals. It may be used for prevention after a needlestick injury or other potential exposure. However, it is not a first-line treatment. It is given by mouth.

Lamivudine, commonly called 3TC, is an antiretroviral medication used to prevent and treat HIV/AIDS. It is also used to treat chronic hepatitis B when other options are not possible. It is effective against both HIV-1 and HIV-2. It is typically used in combination with other antiretrovirals such as zidovudine, dolutegravir, and abacavir. Lamivudine may be included as part of post-exposure prevention in those who have been potentially exposed to HIV. Lamivudine is taken by mouth as a liquid or tablet.

Nevirapine (NVP), sold under the brand name Viramune among others, is a medication used to treat and prevent HIV/AIDS, specifically HIV-1. It is generally recommended for use with other antiretroviral medications. It may be used to prevent mother to child spread during birth but is not recommended following other exposures. It is taken by mouth.
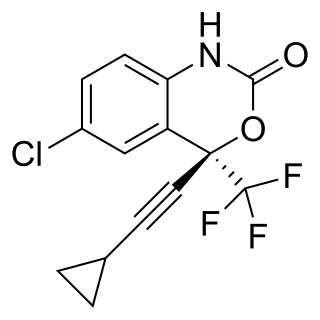
Efavirenz (EFV), sold under the brand names Sustiva among others, is an antiretroviral medication used to treat and prevent HIV/AIDS. It is generally recommended for use with other antiretrovirals. It may be used for prevention after a needlestick injury or other potential exposure. It is sold both by itself and in combination as efavirenz/emtricitabine/tenofovir. It is taken by mouth.

Darunavir (DRV), sold under the brand name Prezista among others, is an antiretroviral medication used to treat and prevent HIV/AIDS. It is generally recommended for use with other antiretrovirals. It is often used with low doses of ritonavir or cobicistat to increase darunavir levels. It may be used for prevention after a needlestick injury or other potential exposure. It is taken by mouth once to twice a day.
Human immunodeficiency virus (HIV) and hepatitis C virus (HCV) co-infection is a multi-faceted, chronic condition that significantly impacts public health. According to the World Health Organization (WHO), 2 to 15% of those infected with HIV are also affected by HCV, increasing their risk of morbidity and mortality due to accelerated liver disease. The burden of co-infection is especially high in certain high-risk groups, such as intravenous drug users and men who have sex with men. These individuals who are HIV-positive are commonly co-infected with HCV due to shared routes of transmission including, but not limited to, exposure to HIV-positive blood, sexual intercourse, and passage of the Hepatitis C virus from mother to infant during childbirth.
HIV superinfection is a condition in which a person with an established human immunodeficiency virus infection acquires a second strain of HIV, often of a different subtype. These can form a recombinant strain that co-exists with the strain from the initial infection, as well from reinfection with a new virus strain, and may cause more rapid disease progression or carry multiple resistances to certain HIV medications.

A resistance mutation is a mutation in a virus gene that allows the virus to become resistant to treatment with a particular antiviral drug. The term was first used in the management of HIV, the first virus in which genome sequencing was routinely used to look for drug resistance. At the time of infection, a virus will infect and begin to replicate within a preliminary cell. As subsequent cells are infected, random mutations will occur in the viral genome. When these mutations begin to accumulate, antiviral methods will kill the wild type strain, but will not be able to kill one or many mutated forms of the original virus. At this point a resistance mutation has occurred because the new strain of virus is now resistant to the antiviral treatment that would have killed the original virus. Resistance mutations are evident and widely studied in HIV due to its high rate of mutation and prevalence in the general population. Resistance mutation is now studied in bacteriology and parasitology.
The cost of HIV treatment is a complicated issue with an extremely wide range of costs due to varying factors such as the type of antiretroviral therapy and the country in which the treatment is administered. The first line therapy of HIV, or the initial antiretroviral drug regimen for an HIV-infected patient, is generally cheaper than subsequent second-line or third-line therapies. There is also a great variability of drug prices among low, middle, and high income countries. In general, low-income countries have the lowest cost of antiretroviral therapy, while middle- and high-income tend to have considerably higher costs. Certain prices of HIV drugs may be high and difficult to afford due to patent barriers on antiretroviral drugs and slow regulatory approval for drugs, which may lead to indirect consequences such as greater HIV drug resistance and an increased number of opportunistic infections. Government and activist movements have taken efforts to limit the price of HIV drugs.
The Berlin patient is an anonymous person from Berlin, Germany, who was described in 1998 as exhibiting prolonged "post-treatment control" of HIV viral load after HIV treatments were interrupted.
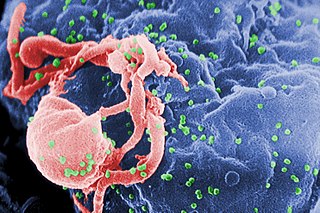
HIV/AIDS research includes all medical research that attempts to prevent, treat, or cure HIV/AIDS, as well as fundamental research about the nature of HIV as an infectious agent and AIDS as the disease caused by HIV.

Fostemsavir, sold under the brand name Rukobia, is an antiretroviral medication for adults living with HIV/AIDS who have tried multiple HIV medications and whose HIV infection cannot be successfully treated with other therapies because of resistance, intolerance or safety considerations.
HIV in pregnancy is the presence of an HIV/AIDS infection in a woman while she is pregnant. There is a risk of HIV transmission from mother to child in three primary situations: pregnancy, childbirth, and while breastfeeding. This topic is important because the risk of viral transmission can be significantly reduced with appropriate medical intervention, and without treatment HIV/AIDS can cause significant illness and death in both the mother and child. This is exemplified by data from The Centers for Disease Control (CDC): In the United States and Puerto Rico between the years of 2014–2017, where prenatal care is generally accessible, there were 10,257 infants in the United States and Puerto Rico who were exposed to a maternal HIV infection in utero who did not become infected and 244 exposed infants who did become infected.
Treatment as prevention (TasP) is a concept in public health that promotes treatment as a way to prevent and reduce the likelihood of HIV illness, death and transmission from an infected individual to others. Expanding access to earlier HIV diagnosis and treatment as a means to address the global epidemic by preventing illness, death and transmission was first proposed in 2000 by Garnett et al. The term is often used to talk about treating people that are currently living with human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) to prevent illness, death and transmission. Although some experts narrow this to only include preventing infections, treatment prevents illnesses such as tuberculosis and has been shown to prevent death. In relation to HIV, antiretroviral therapy (ART) is a three or more drug combination therapy that is used to decrease the viral load, or the measured amount of virus, in an infected individual. Such medications are used as a preventative for infected individuals to not only spread the HIV virus to their negative partners but also improve their current health to increase their lifespans. When taken correctly, ART is able to diminish the presence of the HIV virus in the bodily fluids of an infected person to a level of undetectability. Consistent adherence to an ARV regimen, monitoring, and testing are essential for continued confirmed viral suppression. Treatment as prevention rose to great prominence in 2011, as part of the HPTN 052 study, which shed light on the benefits of early treatment for HIV positive individuals.
Viral load monitoring for HIV is the regular measurement of the viral load of individual HIV-positive people as part of their personal plan for treatment of HIV/AIDS. A count of the viral load is routine before the start of HIV treatment.

Bictegravir/emtricitabine/tenofovir alafenamide, sold under the brand name Biktarvy, is a fixed-dose combination antiretroviral medication for the treatment of HIV/AIDS. It contains bictegravir, a human immunodeficiency virus type 1 (HIV-1) integrase strand transfer inhibitor; emtricitabine, an HIV-1 nucleoside analog reverse transcriptase inhibitor; and tenofovir alafenamide, an HIV-1 nucleoside analog reverse transcriptase inhibitor.
Semzuvolimab, formerly known as UB-421 is an experimental HIV antibody, under development by United Biomedical, Inc. (UBI), headquartered in Hauppauge, New York, U.S. for use in the treatment of HIV infection. By blocking the CDR2 domain of the CD4 receptor of the virus, it prevents initial viral attachment to the host T cell and entry into the host immune cell via a competitive inhibition mechanism. The antibody is unlikely to promote resistance to itself via generation of CD4-independent virus, and has performed well in phase 2 open-label trials. Additionally, it offers hope to HIV patients whose infection has become multi-drug resistant. Furthermore, the antibody has shown long term suppression, which requires the patient to be treated less often, which improves treatment adherence. Previous experimental infusions of broadly neutralizing antibodies (bNABs) have suppressed HIV for about two weeks by targeting proteins on the virus itself, but the rapid mutation rate of HIV induces antibody-resistant strains that render the treatment ineffective. UB-421 theoretically avoids this possibility by blocking a stable human protein that HIV uses to infect T cells. Its advantages include its competitive inhibition, a high affinity of UB-421 to CD4 T cells which is 100 times stronger than HIV, its neutralization of multiple sub-types of HIV, its inhibition of both cell-to-cell and cell-free transmission of HIV, and its immune modulation of training the immune system to better attack HIV, all of which provide potential as monotherapy.

Lenacapavir, sold under the brand name Sunlenca, is an antiretroviral medication used to treat HIV/AIDS. It is taken by mouth or by subcutaneous injection.
References
- ↑ Larder B (2001). "Mechanisms of HIV-1 drug resistance". AIDS. 15 Suppl 5: S27–34. doi: 10.1097/00002030-200100005-00005 . PMID 11816171.
- ↑ "HIV and drug resistance". unaids.org. Retrieved 30 October 2018.
- 1 2 3 HIV drug resistance report 2017. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO.
- ↑ "Antiretroviral Drug Discovery and Development". National Institute of Allergy and Infectious Diseases. Retrieved 25 October 2018.
- 1 2 3 Freeman S, Herron JC (2007). "Evolutionary Analysis.". A case for evolutionary thinking: understanding HIV (4th ed.). San Francisco, CA: Pearson Benjamin Cummings.
- ↑ "Treatment Goals Adult and Adolescent ARV". AIDSinfo. Archived from the original on 31 August 2020. Retrieved 9 November 2018.
- 1 2 "Drug Resistance". AIDSinfo. U.S. Department of Health and Human Services. Retrieved 31 October 2017.
- 1 2 Clavel F, Hance AJ (March 2004). "HIV drug resistance". The New England Journal of Medicine. 350 (10): 1023–35. doi:10.1056/nejmra025195. PMID 14999114.
- ↑ Kozal MJ (January 2009). "Drug-resistant human immunodefiency virus". Clinical Microbiology and Infection. 15 Suppl 1: 69–73. doi: 10.1111/j.1469-0691.2008.02687.x . PMID 19220361.
- 1 2 Pascu ML (2017). Laser Optofluidics in Fighting Multiple Drug Resistance. Bentham Science Publishers. p. 119.
- ↑ "Mechanisms of HIV-1 drug resistance : AIDS". LWW. Retrieved 30 October 2018.
- 1 2 Nachega JB, Marconi VC, van Zyl GU, Gardner EM, Preiser W, Hong SY, Mills EJ, Gross R (April 2011). "HIV treatment adherence, drug resistance, virologic failure: evolving concepts". Infectious Disorders Drug Targets. 11 (2): 167–74. doi:10.2174/187152611795589663. PMC 5072419 . PMID 21406048.
- ↑ "Adherence Limitations to Treatment Safety and Efficacy Adult and Adolescent ARV". AIDSinfo. Retrieved 9 November 2018.
- ↑ Richman DD, Morton SC, Wrin T, Hellmann N, Berry S, Shapiro MF, Bozzette SA (July 2004). "The prevalence of antiretroviral drug resistance in the United States". AIDS. 18 (10): 1393–401. doi: 10.1097/01.aids.0000131310.52526.c7 . PMID 15199315. S2CID 15960179.
- ↑ Choi JY, Kwon OK, Choi BS, Kee MK, Park M, Kim SS (June 2014). "The prevalence of antiretroviral multidrug resistance in highly active antiretroviral therapy-treated patients with HIV/AIDS between 2004 and 2009 in South Korea". Journal of Clinical Virology. 60 (2): 154–60. doi:10.1016/j.jcv.2014.02.004. PMID 24680255.
- ↑ "HIV drug resistance report. Geneva: World Health Organization; 2017. Licence: CC BY-NC-SA 3.0 IGO" (PDF).
- ↑ "Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection". World Health Organization. Retrieved 1 November 2017.
- 1 2 3 Gilks CF, Crowley S, Ekpini R, Gove S, Perriens J, Souteyrand Y, Sutherland D, Vitoria M, Guerma T, De Cock K (August 2006). "The WHO public-health approach to antiretroviral treatment against HIV in resource-limited settings". Lancet. 368 (9534): 505–10. doi:10.1016/S0140-6736(06)69158-7. PMID 16890837. S2CID 22499739.
- ↑ "Global action plan on HIV drug resistance 2017–2021". World Health Organization. Archived from the original on 23 July 2017. Retrieved 1 November 2017.
- ↑ Cane PA (September 2009). "New developments in HIV drug resistance". The Journal of Antimicrobial Chemotherapy. 64 Suppl 1: i37–40. doi: 10.1093/jac/dkp258 . PMID 19675018.
- 1 2 Rosenberg T (28 January 2001). "Look at Brazil". The New York Times. Retrieved 9 November 2018.
- ↑ Dugger CW (29 November 2003). "Rural Haitians Are Vanguard in AIDS Battle". The New York Times. Retrieved 25 October 2018.
- ↑ "WHO urges action against HIV drug resistance threat". World Health Organization. Retrieved 25 October 2018.
- ↑ "Antiretroviral Drug Discovery and Development | NIH: National Institute of Allergy and Infectious Diseases". niaid.nih.gov. Retrieved 25 October 2018.
- ↑ "HIV and drug resistance". unaids.org. Retrieved 30 October 2018.