The maxilla in vertebrates is the upper fixed bone of the jaw formed from the fusion of two maxillary bones. In humans, the upper jaw includes the hard palate in the front of the mouth. The two maxillary bones are fused at the intermaxillary suture, forming the anterior nasal spine. This is similar to the mandible, which is also a fusion of two mandibular bones at the mandibular symphysis. The mandible is the movable part of the jaw.

Rhinoplasty, commonly called nose job, medically called nasal reconstruction is a plastic surgery procedure for altering and reconstructing the nose. There are two types of plastic surgery used – reconstructive surgery that restores the form and functions of the nose and cosmetic surgery that changes the appearance of the nose. Reconstructive surgery seeks to resolve nasal injuries caused by various traumas including blunt, and penetrating trauma and trauma caused by blast injury. Reconstructive surgery can also treat birth defects, breathing problems, and failed primary rhinoplasties. Rhinoplasty may remove a bump, narrow nostril width, change the angle between the nose and the mouth, or address injuries, birth defects, or other problems that affect breathing, such as a deviated nasal septum or a sinus condition. Surgery only on the septum is called a septoplasty.

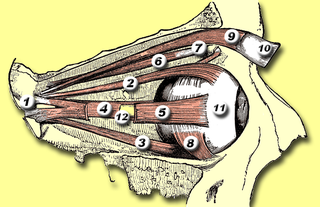
In anatomy, the orbit is the cavity or socket/hole of the skull in which the eye and its appendages are situated. "Orbit" can refer to the bony socket, or it can also be used to imply the contents. In the adult human, the volume of the orbit is 30 millilitres, of which the eye occupies 6.5 ml. The orbital contents comprise the eye, the orbital and retrobulbar fascia, extraocular muscles, cranial nerves II, III, IV, V, and VI, blood vessels, fat, the lacrimal gland with its sac and duct, the eyelids, medial and lateral palpebral ligaments, cheek ligaments, the suspensory ligament, septum, ciliary ganglion and short ciliary nerves.

Eye surgery, also known as ophthalmic surgery or ocular surgery, is surgery performed on the eye or its adnexa. Eye surgery is part of ophthalmology and is performed by an ophthalmologist or eye surgeon. The eye is a fragile organ, and requires due care before, during, and after a surgical procedure to minimize or prevent further damage. An eye surgeon is responsible for selecting the appropriate surgical procedure for the patient, and for taking the necessary safety precautions. Mentions of eye surgery can be found in several ancient texts dating back as early as 1800 BC, with cataract treatment starting in the fifth century BC. It continues to be a widely practiced class of surgery, with various techniques having been developed for treating eye problems.
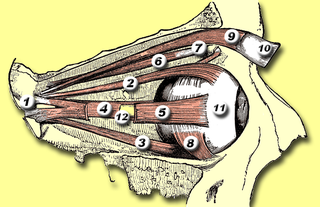
The medial rectus muscle is a muscle in the orbit near the eye. It is one of the extraocular muscles. It originates from the common tendinous ring, and inserts into the anteromedial surface of the eye. It is supplied by the inferior division of the oculomotor nerve (III). It rotates the eye medially (adduction).

The superior orbital fissure is a foramen or cleft of the skull between the lesser and greater wings of the sphenoid bone. It gives passage to multiple structures, including the oculomotor nerve, trochlear nerve, ophthalmic nerve, abducens nerve, ophthalmic veins, and sympathetic fibres from the cavernous plexus.

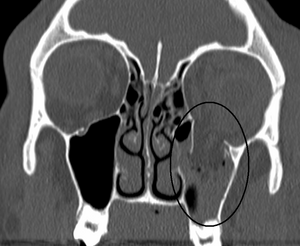
The pyramid-shaped maxillary sinus is the largest of the paranasal sinuses, located in the maxilla. It drains into the middle meatus of the nose through the semilunar hiatus. It is located to the side of the nasal cavity, and below the orbit.
The cavernous sinus within the human head is one of the dural venous sinuses creating a cavity called the lateral sellar compartment bordered by the temporal bone of the skull and the sphenoid bone, lateral to the sella turcica.
Silent sinus syndrome is a spontaneous, asymptomatic collapse of an air sinus associated with negative sinus pressures. It can cause painless facial asymmetry, diplopia and enophthalmos. Diagnosis is suspected based on symptoms, and can be confirmed using a CT scan. Treatment is surgical involving making an outlet for mucous drainage from the obstructed sinus, and, in some cases, paired with reconstruction of the orbital floor. It is slightly more common in middle age.

Functional endoscopic sinus surgery (FESS) is a procedure that is used to treat sinusitis and other conditions that affect the sinuses. Sinusitis is an inflammation of the sinuses that can cause symptoms such as congestion, headaches, and difficulty breathing through the nose.

The human nose is the most protruding part of the face. It bears the nostrils and is the first organ of the respiratory system. It is also the principal organ in the olfactory system. The shape of the nose is determined by the nasal bones and the nasal cartilages, including the nasal septum which separates the nostrils and divides the nasal cavity into two. On average, the nose of a male is larger than that of a female.

A Le Fort fracture of the skull is a classic transfacial fracture of the midface, involving the maxillary bone and surrounding structures in either a horizontal, pyramidal or transverse direction. The hallmark of Lefort fractures is traumatic pterygomaxillary separation, which signifies fractures between the pterygoid plates, horseshoe-shaped bony protuberances which extend from the inferior margin of the maxilla, and the maxillary sinuses. Continuity of this structure is a keystone for stability of the midface, involvement of which impacts surgical management of trauma victims, as it requires fixation to a horizontal bar of the frontal bone. The pterygoid plates lie posterior to the upper dental row, or alveolar ridge, when viewing the face from an anterior view. The fractures are named after French surgeon René Le Fort (1869–1951), who discovered the fracture patterns by examining crush injuries in cadavers.
Endoscopic endonasal surgery is a minimally invasive technique used mainly in neurosurgery and otolaryngology. A neurosurgeon or an otolaryngologist, using an endoscope that is entered through the nose, fixes or removes brain defects or tumors in the anterior skull base. Normally an otolaryngologist performs the initial stage of surgery through the nasal cavity and sphenoid bone; a neurosurgeon performs the rest of the surgery involving drilling into any cavities containing a neural organ such as the pituitary gland. The use of endoscope was first introduced in Transsphenoidal Pituitary Surgery by R Jankowsky, J Auque, C Simon et al. in 1992 G.
Antral lavage is a largely obsolete surgical procedure in which a cannula is inserted into the maxillary sinus via the inferior meatus to allow irrigation and drainage of the sinus. It is also called proof puncture, as the presence of an infection can be proven during the procedure. Upon presence of infection, it can be considered as therapeutic puncture. Often, multiple repeated lavages are subsequently required to allow for full washout of infection.

The zygomaticomaxillary complex fracture, also known as a quadripod fracture, quadramalar fracture, and formerly referred to as a tripod fracture or trimalar fracture, has four components, three of which are directly related to connections between the zygoma and the face, and the fourth being the orbital floor. Its specific locations are the lateral orbital wall, separation of the maxilla and zygoma at the anterior maxilla, the zygomatic arch, and the orbital floor near the infraorbital canal.
Caldwell-Luc surgery, Caldwell-Luc operation, also known as Caldwell-Luc antrostomy, and Radical antrostomy, is an operation to remove irreversibly damaged mucosa of the maxillary sinus. It is done when maxillary sinusitis is not cured by medication or other non-invasive technique. The approach is mainly from the anterior wall of the maxilla bone. It was introduced by George Caldwell (1893)and Henry Luc (1897). The maxillary sinus is entered from two separate openings, one in the canine fossa to gain access to the antrum and other in the naso antral wall for drainage.

Frontal sinus trephination is a surgical procedure where in a small opening is made in the floor of the frontal sinus facilitating drainage of its contents. Drainage of the frontal sinus is done through the floor of frontal sinus above the inner canthus.

Orbital emphysema is a medical condition that refers to the trapping of air within the loose subcutaneous around the orbit that is generally characterized by sudden onset swelling and bruising at the impacted eye, with or without deterioration of vision, which the severity depends on the density of air trapped under the orbital soft tissue spaces.

Canthotomy is a surgical procedure where the lateral canthus, or corner, of the eye is cut to relieve the fluid pressure inside or behind the eye, known as intraocular pressure (IOC). The procedure is typically done in emergency situations when the intraocular pressure becomes too high, which can damage the optic nerve and lead to blindness if left untreated.
Nasal surgery is a medical procedure designed to treat various conditions that cause nasal blockages in the upper respiratory tract, for example nasal polyps, inferior turbinate hypertrophy, and chronic rhinosinusitis. It encompasses several types of techniques, including rhinoplasty, septoplasty, sinus surgery, and turbinoplasty, each with its respective postoperative treatments. Furthermore, nasal surgery is also conducted for cosmetic purposes. While there are potential risks and complications associated, the advancement of medical instruments and enhanced surgical skills have helped mitigate them.