Panniculitis is a group of diseases whose hallmark is inflammation of subcutaneous adipose tissue. Symptoms include tender skin nodules, and systemic signs such as weight loss and fatigue.
Bromoderma is a skin condition characterized by an eruption of papules and pustules on the skin. It is caused by hypersensitivity to bromides, such as those found in certain drugs. There is at least one reported case of bromoderma caused by excessive consumption of a soft drink containing brominated vegetable oil.
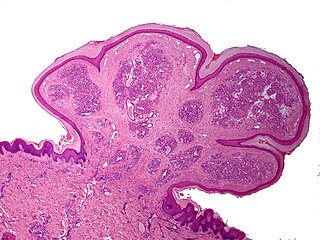
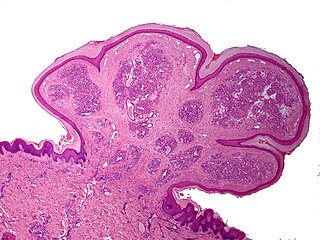
A pyogenic granuloma or lobular capillary hemangioma is a vascular tumor that occurs on both mucosa and skin, and appears as an overgrowth of tissue due to irritation, physical trauma, or hormonal factors. It is often found to involve the gums, skin, or nasal septum, and has also been found far from the head, such as in the thigh.
Atrophia Maculosa Varioliformis Cutis (AMVC) is an idiopathic noninflammatory macular atrophy subtype that affects young people. Clinically, it is distinguished by a variety of shaped, shallow, sharply demaracated depressions.

Elejalde syndrome or neuroectodermal melanolysosomal disease is an extremely rare autosomal recessive syndrome consisting of moderate pigment dilution, profound central nervous system dysfunction, no immune defects, and hair with a metallic silvery sheen. The changes to hair and skin pigmentation are associated with altered melanosome trafficking.
Lupus erythematosus panniculitis presents with subcutaneous nodules that are commonly firm, sharply defined and nontender.
Anetoderma is a benign but uncommon disorder that causes localized areas of flaccid or herniated sac-like skin due to a focal reduction of dermal elastic tissue. Anetoderma is subclassified as primary anetoderma, secondary anetoderma, iatrogenic anetoderma of prematurity, congenital anetoderma, familial anetoderma, and drug-induced anetoderma.
Palisaded neutrophilic and granulomatous dermaititis (PNGS) is usually associated with a well-defined connective tissue disease, lupus erythematosus or rheumatoid arthritis most commonly, and often presents with eroded or ulcerated symmetrically distributed umbilicated papules or nodules on the elbows.
Eccrine angiomatous hamartoma (EAH), first described by Lotzbeck in 1859, is a rare benign vascular hamartoma characterized histologically by a proliferation of eccrine and vascular components. EAH exists on a spectrum of cutaneous tumors that include eccrine nevus, mucinous eccrine nevus and EAH. Each diagnostic subtype is characterized by an increase in the number as well as size of mature eccrine glands or ducts, with EAH being distinguished by the added vascular component.
Congenital smooth muscle hamartoma is typically a skin colored or lightly pigmented patch or plaque with hypertrichosis. Congenital smooth muscle hamartoma was originally reported in 1969 by Sourreil et al.

Annular erythema of infancy(AEI) consists of self-limited eruptions of erythematous, annular to polycyclic patches and plaques. It is an idiopathic figurate erythema. Over several days, a single lesion disappears without leaving behind any scale or hyperpigmentation. Mostly affecting the trunk, face, and extremities, this rash has no symptoms. The diagnosis of AEI is made through a combination of histopathologic and clinical examinations. The disease first manifests in infancy, and if treatment is not received, the periodic eruptions usually stop after the first year of life.
Sclerema neonatorum is a rare and severe skin condition that is characterized by diffuse hardening of the subcutaneous tissue with minimal inflammation.
Self-healing juvenile cutaneous mucinosis is a skin condition caused by fibroblasts producing abnormally large amounts of mucopolysaccharides, and is characterized by the sudden onset of skin lesions and polyarthritis.
Reticular erythematous mucinosis (REM) is a skin condition caused by fibroblasts producing abnormally large amounts of mucopolysaccharides. It is a disease that tends to affect women in the third and fourth decades of life.
Benign cephalic histiocytosis(BCH) is a non-Langerhan's histiocytosis that is uncommon and self-limiting, usually beginning towards the end of the first year of life. Gianotti et al. originally described it in 1971. Initially affecting the head and neck, this condition is characterized by several small eruptions of yellow to reddish-brow papules that heal on their own. Histological investigations have demonstrated that this disorder is associated with dermal proliferation of histiocytes, characterized by intracytoplasmic comma-shaped bodies, covered vesicles, and desmosome-like structure.
Generalized eruptive histiocytoma is a rare cutaneous condition characterized by widespread, erythematous, essentially symmetrical papules, particularly involving the trunk and proximal extremities.

Balloon cell nevus is a benign nevus. It appears like a melanocytic nevus.
Idiopathic facial aseptic granuloma is a cutaneous condition characterized by a chronic, painless, solitary nodule, reminiscent of an acne nodule, appearing on the cheeks of young children. It has a prolonged course, but spontaneously heals.
Symmetrical drug-related intertriginous and flexural exanthema (SDRIFE), popularly known as baboon syndrome because of its resemblance to the distinctive red buttocks displayed by female baboons, is a systemic dermatitis characterized by well-demarcated patches of erythema distributed symmetrically on the buttocks. The cause of the syndrome may be drug-related: i.e., induced by systemic administration of hydroxyzine, penicillin, iodinated radio contrast media, and others.
Granuloma gluteale infantum is a cutaneous condition that appears in the anogenital region of infants as a complication of diaper dermatitis. According to some, no granulomas are found.