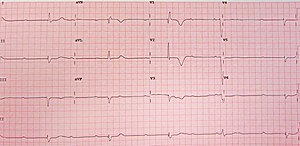
Bradycardia is a slow resting heart rate, commonly under 60 beats per minute (BPM) as determined by an electrocardiogram. It is considered to be a normal heart rate during sleep, in young and healthy or elderly adults, and in athletes.

Electrocardiography is the process of producing an electrocardiogram, a recording of the heart's electrical activity through repeated cardiac cycles. It is an electrogram of the heart which is a graph of voltage versus time of the electrical activity of the heart using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including cardiac rhythm disturbances, inadequate coronary artery blood flow, and electrolyte disturbances.

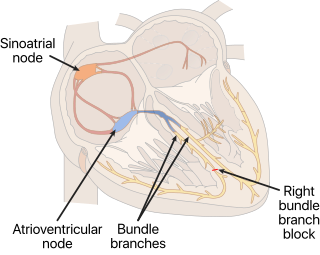
The cardiac conduction system(CCS) (also called the electrical conduction system of the heart) transmits the signals generated by the sinoatrial node – the heart's pacemaker, to cause the heart muscle to contract, and pump blood through the body's circulatory system. The pacemaking signal travels through the right atrium to the atrioventricular node, along the bundle of His, and through the bundle branches to Purkinje fibers in the walls of the ventricles. The Purkinje fibers transmit the signals more rapidly to stimulate contraction of the ventricles.

First-degree atrioventricular block is a disease of the electrical conduction system of the heart in which electrical impulses conduct from the cardiac atria to the ventricles through the atrioventricular node more slowly than normal. First degree AV block does not generally cause any symptoms, but may progress to more severe forms of heart block such as second- and third-degree atrioventricular block. It is diagnosed using an electrocardiogram, and is defined as a PR interval greater than 200 milliseconds. First degree AV block affects 0.65-1.1% of the population with 0.13 new cases per 1000 persons each year.

Second-degree atrioventricular block is a disease of the electrical conduction system of the heart. It is a conduction block between the atria and ventricles. The presence of second-degree AV block is diagnosed when one or more of the atrial impulses fail to conduct to the ventricles due to impaired conduction. It is classified as a block of the AV node and is categorized in between first-degree and third degree blocks.

Ventricular tachycardia is a fast heart rate arising from the lower chambers of the heart. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple episodes over a short period of time are referred to as an electrical storm. Short periods may occur without symptoms, or present with lightheadedness, palpitations, or chest pain. Ventricular tachycardia may result in ventricular fibrillation (VF) and turn into cardiac arrest. This conversion of the VT into VF is called the degeneration of the VT. It is found initially in about 7% of people in cardiac arrest.

Supraventricular tachycardia (SVT) is an umbrella term for fast heart rhythms arising from the upper part of the heart. This is in contrast to the other group of fast heart rhythms – ventricular tachycardia, which start within the lower chambers of the heart. There are four main types of SVT: atrial fibrillation, atrial flutter, paroxysmal supraventricular tachycardia (PSVT), and Wolff–Parkinson–White syndrome. The symptoms of SVT include palpitations, feeling of faintness, sweating, shortness of breath, and/or chest pain.

AV-nodal reentrant tachycardia (AVNRT) is a type of abnormal fast heart rhythm. It is a type of supraventricular tachycardia (SVT), meaning that it originates from a location within the heart above the bundle of His. AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia. It is more common in women than men. The main symptom is palpitations. Treatment may be with specific physical maneuvers, medications, or, rarely, synchronized cardioversion. Frequent attacks may require radiofrequency ablation, in which the abnormally conducting tissue in the heart is destroyed.

A bundle branch block is a defect in one of the bundle branches in the electrical conduction system of the heart.
A right bundle branch block (RBBB) is a heart block in the right bundle branch of the electrical conduction system.

Atrioventricular block is a type of heart block that occurs when the electrical signal traveling from the atria, or the upper chambers of the heart, to ventricles, or the lower chambers of the heart, is impaired. Normally, the sinoatrial node produces an electrical signal to control the heart rate. The signal travels from the SA node to the ventricles through the atrioventricular node. In an AV block, this electrical signal is either delayed or completely blocked. When the signal is completely blocked, the ventricles produce their own electrical signal to control the heart rate. The heart rate produced by the ventricles is much slower than that produced by the SA node.

In cardiology, a ventricular escape beat is a self-generated electrical discharge initiated by, and causing contraction of the ventricles of the heart; normally the heart rhythm is begun in the atria of the heart and is subsequently transmitted to the ventricles. The ventricular escape beat follows a long pause in ventricular rhythm and acts to prevent cardiac arrest. It indicates a failure of the electrical conduction system of the heart to stimulate the ventricles.
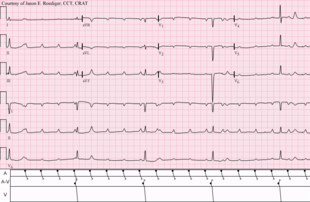
Sinoatrial arrest is a medical condition wherein the sinoatrial node of the heart transiently ceases to generate the electrical impulses that normally stimulate the myocardial tissues to contract and thus the heart to beat. It is defined as lasting from 2.0 seconds to several minutes. Since the heart contains multiple pacemakers, this interruption of the cardiac cycle generally lasts only a few seconds before another part of the heart, such as the atrio-ventricular junction or the ventricles, begins pacing and restores the heart action. This condition can be detected on an electrocardiogram (ECG) as a brief period of irregular length with no electrical activity before either the sinoatrial node resumes normal pacing, or another pacemaker begins pacing. If a pacemaker other than the sinoatrial node is pacing the heart, this condition is known as an escape rhythm. If no other pacemaker begins pacing during an episode of sinus arrest it becomes a cardiac arrest. This condition is sometimes confused with sinoatrial block, a condition in which the pacing impulse is generated, but fails to conduct through the myocardium. Differential diagnosis of the two conditions is possible by examining the exact length of the interruption of cardiac activity. If the next available pacemaker takes over, it is in the following order:

Accelerated idioventricular rhythm is a ventricular rhythm with a rate of between 40 and 120 beats per minute. Idioventricular means “relating to or affecting the cardiac ventricle alone” and refers to any ectopic ventricular arrhythmia. Accelerated idioventricular arrhythmias are distinguished from ventricular rhythms with rates less than 40 and those faster than 120. Though some other references limit to between 60 and 100 beats per minute. It is also referred to as AIVR and "slow ventricular tachycardia."

Junctional rhythm describes an abnormal heart rhythm resulting from impulses coming from a locus of tissue in the area of the atrioventricular node(AV node), the "junction" between atria and ventricles.

A sinoatrial block is a disorder in the normal rhythm of the heart, known as a heart block, that is initiated in the sinoatrial node. The initial action impulse in a heart is usually formed in the sinoatrial node and carried through the atria, down the internodal atrial pathways to the atrioventricular node (AV) node. In normal conduction, the impulse would travel across the bundle of His, down the bundle branches, and into the Purkinje fibers. This would depolarize the ventricles and cause them to contract.

Junctional ectopic tachycardia (JET) is a rare syndrome of the heart that manifests in patients recovering from heart surgery. It is characterized by cardiac arrhythmia, or irregular beating of the heart, caused by abnormal conduction from or through the atrioventricular node. In newborns and infants up to 6 weeks old, the disease may also be referred to as His bundle tachycardia or congenital JET.

In electrocardiography, left axis deviation (LAD) is a condition wherein the mean electrical axis of ventricular contraction of the heart lies in a frontal plane direction between −30° and −90°. This is reflected by a QRS complex positive in lead I and negative in leads aVF and II.
An idioventricular rhythm is a cardiac rhythm characterized by a rate of <50 beats per minute (bpm), absence of P waves and widening of the QRS complex. In cases where the heart rate is between 50 and 110 bpm, it is known as accelerated idioventricular rhythm and ventricular tachycardia if the rate exceeds 120 bpm. Causes of idioventricular rhythms are varied and can include drugs or a heart defect at birth. It is typically benign and not life-threatening.
A tachycardia-dependent bundle branch block is a defect in the conduction system of the heart, and is distinct from typical bundle branch blocks due to its reliable, reproducible onset related to an increase in the rate of cardiac contraction. Tachycardia-dependent bundle branch block can prevent both ventricles from contracting efficiently and can limit the cardiac output of the heart.