Thyroid-stimulating hormone (also known as thyrotropin, thyrotropic hormone, or abbreviated TSH) is a pituitary hormone that stimulates the thyroid gland to produce thyroxine (T4), and then triiodothyronine (T3) which stimulates the metabolism of almost every tissue in the body. It is a glycoprotein hormone produced by thyrotrope cells in the anterior pituitary gland, which regulates the endocrine function of the thyroid.

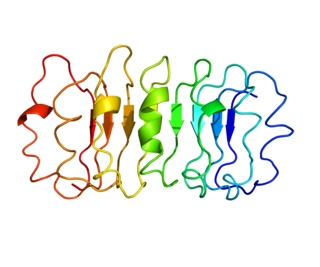
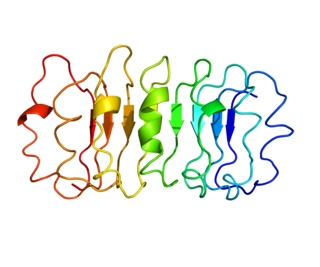
Thyroxine-binding globulin (TBG) is a globulin protein that in humans is encoded by the SERPINA7 gene. TBG binds thyroid hormones in circulation. It is one of three transport proteins (along with transthyretin and serum albumin) responsible for carrying the thyroid hormones thyroxine (T4) and triiodothyronine (T3) in the bloodstream. Of these three proteins, TBG has the highest affinity for T4 and T3 but is present in the lowest concentration relative to transthyretin and albumin, which also bind T3 and T4 in circulation. Despite its low concentration, TBG carries the majority of T4 in the blood plasma. Due to the very low concentration of T4 and T3 in the blood, TBG is rarely more than 25% saturated with its ligand. Unlike transthyretin and albumin, TBG has a single binding site for T4/T3. TBG is synthesized primarily in the liver as a 54-kDa protein. In terms of genomics, TBG is a serpin; however, it has no inhibitory function like many other members of this class of proteins.
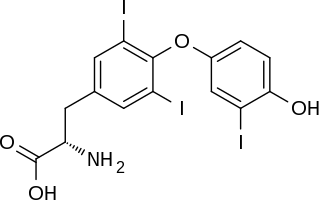
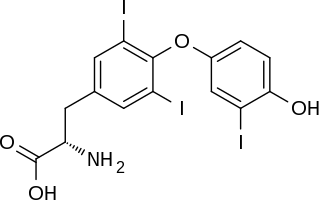
Triiodothyronine, also known as T3, is a thyroid hormone. It affects almost every physiological process in the body, including growth and development, metabolism, body temperature, and heart rate.

Levothyroxine, also known as L-thyroxine, is a manufactured form of the thyroid hormone thyroxine (T4). It is used to treat thyroid hormone deficiency (hypothyroidism), including Hashimoto's disease and a severe form known as myxedema coma. It may also be used to treat and prevent certain types of thyroid tumors. It is not indicated for weight loss. Levothyroxine is taken by mouth or given by intravenous injection. Maximum effect from a specific dose can take up to six weeks to occur.

Thyroid disease is a medical condition that affects the function of the thyroid gland. The thyroid gland is located at the front of the neck and produces thyroid hormones that travel through the blood to help regulate many other organs, meaning that it is an endocrine organ. These hormones normally act in the body to regulate energy use, infant development, and childhood development.
Thyroid function tests (TFTs) is a collective term for blood tests used to check the function of the thyroid. TFTs may be requested if a patient is thought to suffer from hyperthyroidism or hypothyroidism, or to monitor the effectiveness of either thyroid-suppression or hormone replacement therapy. It is also requested routinely in conditions linked to thyroid disease, such as atrial fibrillation and anxiety disorder.
The thyroid hormone receptor (TR) is a type of nuclear receptor that is activated by binding thyroid hormone. TRs act as transcription factors, ultimately affecting the regulation of gene transcription and translation. These receptors also have non-genomic effects that lead to second messenger activation, and corresponding cellular response.
Desiccated thyroid, also known as thyroid extract, is thyroid gland that has been dried and powdered for medical use. It is used to treat hypothyroidism. It is less preferred than levothyroxine. It is taken by mouth. Maximal effects may take up to 3 weeks to occur.
The thyrotropin receptor is a receptor that responds to thyroid-stimulating hormone and stimulates the production of thyroxine (T4) and triiodothyronine (T3). The TSH receptor is a member of the G protein-coupled receptor superfamily of integral membrane proteins and is coupled to the Gs protein.

The hypothalamic–pituitary–thyroid axis is part of the neuroendocrine system responsible for the regulation of metabolism and also responds to stress.
Euthyroid sick syndrome (ESS) is a state of adaptation or dysregulation of thyrotropic feedback control wherein the levels of T3 and/or T4 are abnormal, but the thyroid gland does not appear to be dysfunctional. This condition may result from allostatic responses of hypothalamus-pituitary-thyroid feedback control, dyshomeostatic disorders, drug interferences, and impaired assay characteristics in critical illness.

Gonadotropin-releasing hormone receptor is a protein that in humans is encoded by the GNRHR gene.
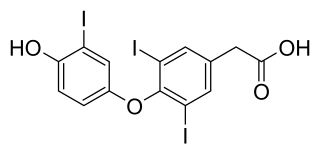
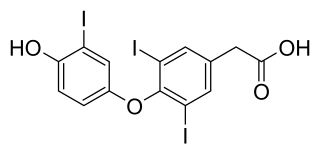
Tiratricol is a thyroid hormone analogue. Triiodothyroacetic acid is also a physiologic thyroid hormone that is present in the normal organism in low concentrations.

Thyroid hormone receptor beta (TR-beta) also known as nuclear receptor subfamily 1, group A, member 2 (NR1A2), is a nuclear receptor protein that in humans is encoded by the THRB gene.

Homeobox protein prophet of PIT-1 is a protein that in humans is encoded by the PROP1 gene.

Thyroid stimulating hormone, beta also known as TSHB is a protein which in humans is encoded by the TSHB gene.

Mild androgen insensitivity syndrome (MAIS) is a condition that results in a mild impairment of the cell's ability to respond to androgens. The degree of impairment is sufficient to impair spermatogenesis and / or the development of secondary sexual characteristics at puberty in males, but does not affect genital differentiation or development. Female genital and sexual development is not significantly affected by the insensitivity to androgens; as such, MAIS is only diagnosed in males. The clinical phenotype associated with MAIS is a normal male habitus with mild spermatogenic defect and / or reduced secondary terminal hair.
The fetal endocrine system is one of the first systems to develop during prenatal development.
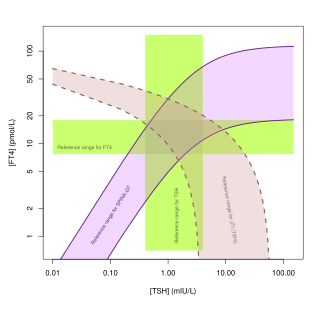
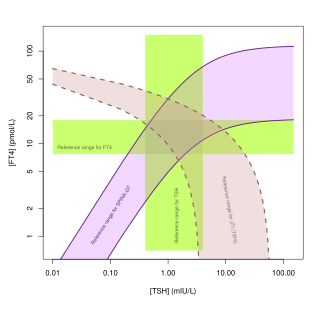
Jostel's TSH index, also referred to as Jostel's thyrotropin index or Thyroid Function index (TFI), is a method for estimating the thyrotropic function of the anterior pituitary lobe in a quantitative way. The equation has been derived from the logarithmic standard model of thyroid homeostasis. In a paper from 2014 further study was suggested to show if it is useful, but the 2018 guideline by the European Thyroid Association for the diagnosis of uncertain cases of central hypothyroidism regarded it as beneficial.
The Thyrotroph Thyroid Hormone Sensitivity Index is a calculated structure parameter of thyroid homeostasis. It was originally developed to deliver a method for fast screening for resistance to thyroid hormone. Today it is also used to get an estimate for the set point of thyroid homeostasis, especially to assess dynamic thyrotropic adaptation of the anterior pituitary gland, including non-thyroidal illnesses.