Addison's disease, also known as primary adrenal insufficiency, is a rare long-term endocrine disorder characterized by inadequate production of the steroid hormones cortisol and aldosterone by the two outer layers of the cells of the adrenal glands, causing adrenal insufficiency. Symptoms generally come on slowly and insidiously and may include abdominal pain and gastrointestinal abnormalities, weakness, and weight loss. Darkening of the skin in certain areas may also occur. Under certain circumstances, an adrenal crisis may occur with low blood pressure, vomiting, lower back pain, and loss of consciousness. Mood changes may also occur. Rapid onset of symptoms indicates acute adrenal failure, which is a clinical emergency. An adrenal crisis can be triggered by stress, such as from an injury, surgery, or infection.

Adrenal insufficiency is a condition in which the adrenal glands do not produce adequate amounts of steroid hormones. The adrenal glands—also referred to as the adrenal cortex—normally secrete glucocorticoids, mineralocorticoids, and androgens. These hormones are important in regulating blood pressure, electrolytes, and metabolism as a whole. Deficiency of these hormones leads to symptoms ranging from abdominal pain, vomiting, muscle weakness and fatigue, low blood pressure, depression, mood and personality changes to organ failure and shock. Adrenal crisis may occur if a person having adrenal insufficiency experiences stresses, such as an accident, injury, surgery, or severe infection; this is a life-threatening medical condition resulting from severe deficiency of cortisol in the body. Death may quickly follow.
Immunodeficiency, also known as immunocompromisation, is a state in which the immune system's ability to fight infectious diseases and cancer is compromised or entirely absent. Most cases are acquired ("secondary") due to extrinsic factors that affect the patient's immune system. Examples of these extrinsic factors include HIV infection and environmental factors, such as nutrition. Immunocompromisation may also be due to genetic diseases/flaws such as SCID.

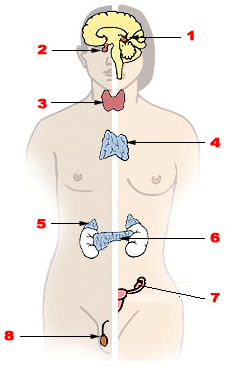
Autoimmune polyendocrine syndromes (APSs), also called polyglandular autoimmune syndromes (PGASs) or polyendocrine autoimmune syndromes (PASs), are a heterogeneous group of rare diseases characterized by autoimmune activity against more than one endocrine organ, although non-endocrine organs can be affected. There are three types of APS, and there are a number of other diseases which involve endocrine autoimmunity.

FOXP3, also known as scurfin, is a protein involved in immune system responses. A member of the FOX protein family, FOXP3 appears to function as a master regulator of the regulatory pathway in the development and function of regulatory T cells. Regulatory T cells generally turn the immune response down. In cancer, an excess of regulatory T cell activity can prevent the immune system from destroying cancer cells. In autoimmune disease, a deficiency of regulatory T cell activity can allow other autoimmune cells to attack the body's own tissues.

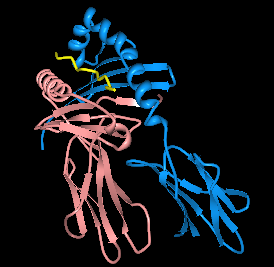
Cytotoxic T-lymphocyte associated protein 4, (CTLA-4) also known as CD152, is a protein receptor that functions as an immune checkpoint and downregulates immune responses. CTLA-4 is constitutively expressed in regulatory T cells but only upregulated in conventional T cells after activation – a phenomenon which is particularly notable in cancers. It acts as an "off" switch when bound to CD80 or CD86 on the surface of antigen-presenting cells. It is encoded by the gene CTLA4 in humans.

Barakat syndrome is a rare disease characterized by hypoparathyroidism, sensorineural deafness and renal disease, and hence also known as HDR syndrome. It is an autosomal dominant condition with incomplete penetrance and variable expressivity that was first described by Amin J. Barakat et al. in 1977.

Immunodysregulation polyendocrinopathy enteropathy X-linked syndrome is a rare autoimmune disease. It is one of the autoimmune polyendocrine syndromes. Most often, IPEX presents with autoimmune enteropathy, dermatitis (eczema), and autoimmune endocrinopathy, but other presentations exist.
Immune dysregulation is any proposed or confirmed breakdown or maladaptive change in molecular control of immune system processes. For example, dysregulation is a component in the pathogenesis of autoimmune diseases and some cancers. Immune system dysfunction, as seen in IPEX syndrome leads to immune dysfunction, polyendocrinopathy, enteropathy, X-linked (IPEX). IPEX typically presents during the first few months of life with diabetes mellitus, intractable diarrhea, failure to thrive, eczema, and hemolytic anemia. unrestrained or unregulated immune response.

The autoimmune regulator (AIRE) is a protein that in humans is encoded by the AIRE gene. It is a 13kb gene on chromosome 21q22.3 that has 545 amino acids. AIRE is a transcription factor expressed in the medulla of the thymus. It is part of the mechanism which eliminates self-reactive T cells that would cause autoimmune disease. It exposes T cells to normal, healthy proteins from all parts of the body, and T cells that react to those proteins are destroyed.
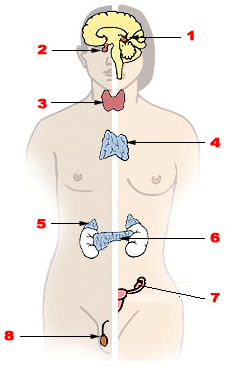
Endocrine diseases are disorders of the endocrine system. The branch of medicine associated with endocrine disorders is known as endocrinology.
The enzyme sialate O-acetylesterase (EC 3.1.1.53) catalyzes the reaction

EEM syndrome is an autosomal recessive congenital malformation disorder affecting tissues associated with the ectoderm, and also the hands, feet and eyes.
Autoimmune polyendocrine syndrome type 2, a form of autoimmune polyendocrine syndrome also known as APS-II, or PAS II, is the most common form of the polyglandular failure syndromes. PAS II is defined as the association between autoimmune Addison's disease and either autoimmune thyroid disease, type 1 diabetes, or both. It is heterogeneous and has not been linked to one gene. Rather, individuals are at a higher risk when they carry a particular human leukocyte antigen. APS-II affects women to a greater degree than men.

Autoimmune enteropathy is a rare autoimmune disorder characterized by weight loss from malabsorption, severe and protracted diarrhea, and autoimmune damage to the intestinal mucosa. Autoimmune enteropathy typically occurs in infants and younger children however, adult cases have been reported in literature. Autoimmune enteropathy was first described by Walker-Smith et al. in 1982.

Rajesh Vasantlal Thakker is May Professor of Medicine in the Nuffield Department of Clinical Medicine at the University of Oxford and a fellow of Somerville College, Oxford. Thakker is also a Consultant physician at the Churchill Hospital and the John Radcliffe Hospital, Principal investigator (PI) at the Oxford Centre for Diabetes, Endocrinology and Metabolism (OCDEM) and was Chairman of the NIHR/MRC Efficacy and Mechanism Evaluation (EME) Board until Spring 2016.
Autoimmune polyendocrine syndrome, type 3 is characterized by the coexistence of two autoimmune illnesses, not including Addison's disease, and an autoimmune thyroid disease. Based on other organ-specific autoimmune involvement, there are multiple subtypes that are classified: type 3a shows thyroid autoimmune disease in conjunction with type 1 diabetes, type 3b shows thyroid autoimmune disease in conjunction with pernicious anemia (PA), and type 3c shows thyroid autoimmune disease in conjunction with alopecia, vitiligo, or other organ-specific autoimmune disease.
STAT3 gain-of function (GOF) is a rare genetic disorder of the immune system, leading to early-onset autoimmunity and a variety of multi-organ disorders. The condition is progressive and manifests through a broad spectrum of clinical symptoms, including lymphadenopathy, autoimmune cytopenias, growth delays, enteropathy, lung disease, endocrine disorders, arthritis, autoimmune hepatitis, neurological diseases, vasculopathy, eczema, infections, and multiorgan autoimmunity. Patients experience recurring infections.
Autoimmunity refers to a pathological immune response of the body's immune system against itself. Autoimmune disease is widely recognized to be significantly more common in women than in men, and often presents differently between the sexes. The reasons for these disparities are still under investigation, but may in part involve the presence of an additional X chromosome in women, as well as the higher presence of female sex hormones such as estrogen. The risk, incidence, and character of autoimmune disease in women may also be associated with female-specific physiological changes, such as hormonal shifts during menses, pregnancy, and menopause.