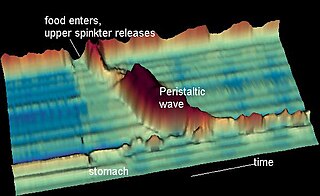
Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver. The digestive system functions to move material through the GI tract via peristalsis, break down that material via digestion, absorb nutrients for use throughout the body, and remove waste from the body via defecation. Physicians who specialize in the medical specialty of gastroenterology are called gastroenterologists or sometimes GI doctors. Some of the most common conditions managed by gastroenterologists include gastroesophageal reflux disease, gastrointestinal bleeding, irritable bowel syndrome, inflammatory bowel disease (IBD) which includes Crohn's disease and ulcerative colitis, peptic ulcer disease, gallbladder and biliary tract disease, hepatitis, pancreatitis, colitis, colon polyps and cancer, nutritional problems, and many more.

Esophageal achalasia, often referred to simply as achalasia, is a failure of smooth muscle fibers to relax, which can cause the lower esophageal sphincter to remain closed. Without a modifier, "achalasia" usually refers to achalasia of the esophagus. Achalasia can happen at various points along the gastrointestinal tract; achalasia of the rectum, for instance, may occur in Hirschsprung's disease. The lower esophageal sphincter is a muscle between the esophagus and stomach that opens when food comes in. It closes to avoid stomach acids from coming back up. A fully understood cause to the disease is unknown, as are factors that increase the risk of its appearance. Suggestions of a genetically transmittable form of achalasia exist, but this is neither fully understood, nor agreed upon.
Heartburn, also known as pyrosis, cardialgia or acid indigestion, is a burning sensation in the central chest or upper central abdomen. Heartburn is usually due to regurgitation of gastric acid into the esophagus. It is the major symptom of gastroesophageal reflux disease (GERD).

Gastroesophageal reflux disease (GERD) or gastro-oesophageal reflux disease (GORD) is a chronic upper gastrointestinal disease in which stomach content persistently and regularly flows up into the esophagus, resulting in symptoms and/or complications. Symptoms include dental corrosion, dysphagia, heartburn, odynophagia, regurgitation, non-cardiac chest pain, extraesophageal symptoms such as chronic cough, hoarseness, reflux-induced laryngitis, or asthma. In the long term, and when not treated, complications such as esophagitis, esophageal stricture, and Barrett's esophagus may arise.

Barrett's esophagus is a condition in which there is an abnormal (metaplastic) change in the mucosal cells lining the lower portion of the esophagus, from stratified squamous epithelium to simple columnar epithelium with interspersed goblet cells that are normally present only in the small intestine and large intestine. This change is considered to be a premalignant condition because it is associated with a high incidence of further transition to esophageal adenocarcinoma, an often-deadly cancer.

Esophagitis, also spelled oesophagitis, is a disease characterized by inflammation of the esophagus. The esophagus is a tube composed of a mucosal lining, and longitudinal and circular smooth muscle fibers. It connects the pharynx to the stomach; swallowed food and liquids normally pass through it.

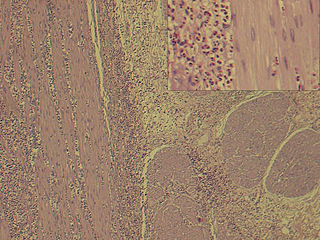
Eosinophils, sometimes called eosinophiles or, less commonly, acidophils, are a variety of white blood cells and one of the immune system components responsible for combating multicellular parasites and certain infections in vertebrates. Along with mast cells and basophils, they also control mechanisms associated with allergy and asthma. They are granulocytes that develop during hematopoiesis in the bone marrow before migrating into blood, after which they are terminally differentiated and do not multiply.

Eosinophilia is a condition in which the eosinophil count in the peripheral blood exceeds 5×108/L (500/μL). Hypereosinophilia is an elevation in an individual's circulating blood eosinophil count above 1.5 × 109/L (i.e. 1,500/μL). The hypereosinophilic syndrome is a sustained elevation in this count above 1.5 × 109/L (i.e. 1,500/μL) that is also associated with evidence of eosinophil-based tissue injury.
Coffee ground vomitus refers to a particular appearance of vomit. Within organic heme molecules of red blood cells is the element iron, which oxidizes following exposure to gastric acid. This reaction causes the vomitus to look like ground coffee.
Esophageal dysphagia is a form of dysphagia where the underlying cause arises from the body of the esophagus, lower esophageal sphincter, or cardia of the stomach, usually due to mechanical causes or motility problems.
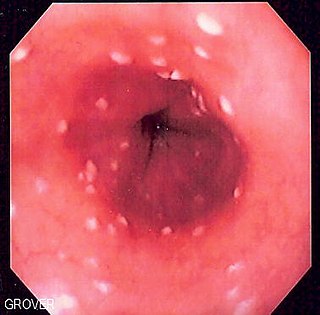
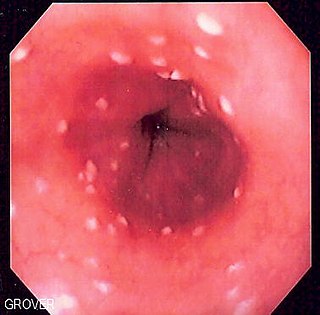
Esophageal candidiasis is an opportunistic infection of the esophagus by Candida albicans. The disease usually occurs in patients in immunocompromised states, including post-chemotherapy and in AIDS. However, it can also occur in patients with no predisposing risk factors, and is more likely to be asymptomatic in those patients. It is also known as candidal esophagitis or monilial esophagitis.
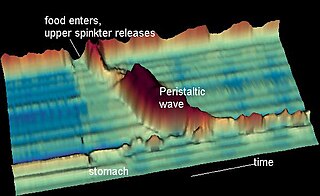
Nutcracker esophagus, jackhammer esophagus, or hypercontractile peristalsis, is a disorder of the movement of the esophagus characterized by contractions in the smooth muscle of the esophagus in a normal sequence but at an excessive amplitude or duration. Nutcracker esophagus is one of several motility disorders of the esophagus, including achalasia and diffuse esophageal spasm. It causes difficulty swallowing, or dysphagia, with both solid and liquid foods, and can cause significant chest pain; it may also be asymptomatic. Nutcracker esophagus can affect people of any age but is more common in the sixth and seventh decades of life.
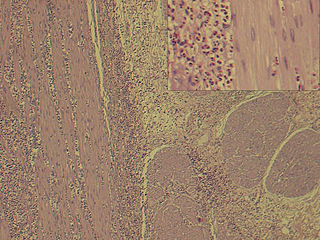
Eosinophilic gastroenteritis, also known as eosinophilic enteritis, is a rare and heterogeneous condition characterized by patchy or diffuse eosinophilic infiltration of gastrointestinal (GI) tissue, first described by Kaijser in 1937. Presentation may vary depending on location as well as depth and extent of bowel wall involvement and usually runs a chronic relapsing course. It can be classified into mucosal, muscular and serosal types based on the depth of involvement. Any part of the GI tract can be affected, and isolated biliary tract involvement has also been reported. The stomach is the organ most commonly affected, followed by the small intestine and the colon.

An esophageal food bolus obstruction is a medical emergency caused by the obstruction of the esophagus by an ingested foreign body.
Cytomegalovirus esophagitis is a form of esophagitis associated with cytomegalovirus. Symptoms include dysphagia, upper abdominal pain, diarrhea, nausea, vomiting, and sometimes hematemesis. This condition occurs in the setting of patients with a weakened immune system who are susceptible to both infections by CMV and the manifestation of symptoms. A large majority of patient that have CMV Esophagitis are diagnosed with HIV. Another significant segment of the population have weakened immune systems through transplant surgery, diabetes, or due to medication. Diagnosis is done primarily by endoscopy with biopsy, as CMV Esophagitis has a distinctive pathology pattern of linear ulcers.

Herpes esophagitis is a viral infection of the esophagus caused by Herpes simplex virus (HSV).

Esophageal intramucosal pseudodiverticulosis (EIPD) is a rare condition wherein the wall of the esophagus develops numerous small outpouchings (pseudodiverticulae). Individuals with the condition typically develop difficulty swallowing. The outpouchings represent the ducts of submucosal glands of the esophagus. It typically affects individuals in their sixth and seventh decades of life. While it is associated with certain chronic conditions, particularly alcoholism, diabetes and gastroesophageal reflux disease, the cause of the condition is unknown. Treatment involves medications to treat concomitant conditions such as reflux and esophageal spasm, and dilation of strictures in the esophagus.

Lymphocytic esophagitis is a rare and poorly understood medical disorder involving inflammation in the esophagus. The disease is named from the primary inflammatory process, wherein lymphocytes are seen within the esophageal mucosa. Symptoms of the condition include difficulty swallowing, heartburn and food bolus obstruction. The condition was first described in 2006 by Rubio and colleagues. Initial reports questioned whether this was a true medical disorder, or whether the inflammation was secondary to another condition, such as gastroesophageal reflux disease.
Esophagogastric junction outflow obstruction (EGJOO) is an esophageal motility disorder characterized by increased pressure where the esophagus connects to the stomach at the lower esophageal sphincter. EGJOO is diagnosed by esophageal manometry. However, EGJOO has a variety of etiologies; evaluating the cause of obstruction with additional testing, such as upper endoscopy, computed tomography, or endoscopic ultrasound may be necessary. When possible, treatment of EGJOO should be directed at the cause of obstruction. When no cause for obstruction is found, observation alone may be considered if symptoms are minimal. Functional EGJOO with significant or refractory symptoms may be treated with pneumatic dilation, per-oral endoscopic myotomy (POEM), or botulinum toxin injection.
Cendakimab is a monoclonal antibody against interleukin 13. It is developed by Bristol Myers Squibb for eosinophilic esophagitis.