Defecation follows digestion, and is a necessary process by which organisms eliminate a solid, semisolid, or liquid waste material known as feces from the digestive tract via the anus or cloaca. The act has a variety of names ranging from the common, like pooping or crapping, to the technical, e.g. bowel movement, to the obscene (shitting), to the euphemistic, to the juvenile. The topic, usually avoided in polite company, can become the basis for some potty humor.

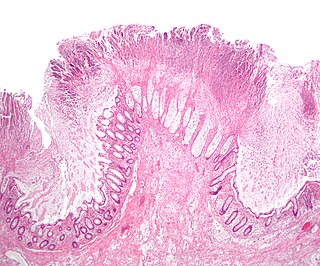
Hirschsprung's disease is a birth defect in which nerves are missing from parts of the intestine. The most prominent symptom is constipation. Other symptoms may include vomiting, abdominal pain, diarrhea and slow growth. Most children develop signs and symptoms shortly after birth. However, others may be diagnosed later in infancy or early childhood. About half of all children with Hirschsprung's disease are diagnosed in the first year of life. Complications may include enterocolitis, megacolon, bowel obstruction and intestinal perforation.

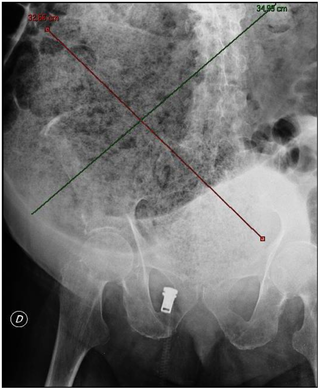
Bowel obstruction, also known as intestinal obstruction, is a mechanical or functional obstruction of the intestines which prevents the normal movement of the products of digestion. Either the small bowel or large bowel may be affected. Signs and symptoms include abdominal pain, vomiting, bloating and not passing gas. Mechanical obstruction is the cause of about 5 to 15% of cases of severe abdominal pain of sudden onset requiring admission to hospital.

Abdominal pain, also known as a stomach ache, is a symptom associated with both non-serious and serious medical issues. Since the abdomen contains most of the body's vital organs, it can be an indicator of a wide variety of diseases. Given that, approaching the examination of a person and planning of a differential diagnosis is extremely important.
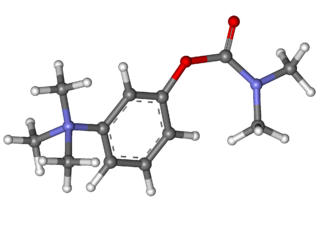
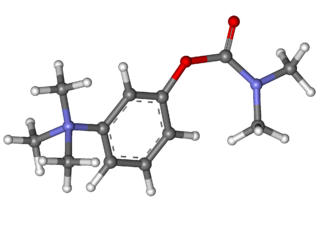
Neostigmine, sold under the brand name Bloxiverz, among others, is a medication used to treat myasthenia gravis, Ogilvie syndrome, and urinary retention without the presence of a blockage. It is also used in anaesthesia to end the effects of non-depolarising neuromuscular blocking medication. It is given by injection either into a vein, muscle, or under the skin. After injection effects are generally greatest within 30 minutes and last up to 4 hours.

Ileus is a disruption of the normal propulsive ability of the intestine. It can be caused by lack of peristalsis or by mechanical obstruction. The word 'ileus' is from Ancient Greek eileós. The term 'subileus' refers to a partial obstruction.
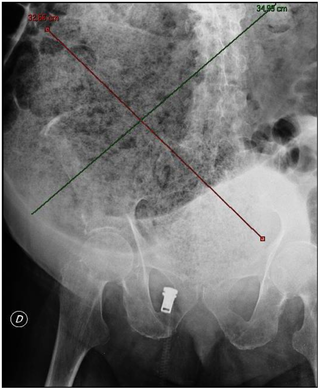
Toxic megacolon is an acute form of colonic distension. It is characterized by a very dilated colon (megacolon), accompanied by abdominal distension (bloating), and sometimes fever, abdominal pain, or shock.
Colic in horses is defined as abdominal pain, but it is a clinical symptom rather than a diagnosis. The term colic can encompass all forms of gastrointestinal conditions which cause pain as well as other causes of abdominal pain not involving the gastrointestinal tract. What makes it tricky is that different causes can manifest with similar signs of distress in the animal. Recognizing and understanding these signs is pivotal, as timely action can spell the difference between a brief moment of discomfort and a life-threatening situation. The most common forms of colic are gastrointestinal in nature and are most often related to colonic disturbance. There are a variety of different causes of colic, some of which can prove fatal without surgical intervention. Colic surgery is usually an expensive procedure as it is major abdominal surgery, often with intensive aftercare. Among domesticated horses, colic is the leading cause of premature death. The incidence of colic in the general horse population has been estimated between 4 and 10 percent over the course of the average lifespan. Clinical signs of colic generally require treatment by a veterinarian. The conditions that cause colic can become life-threatening in a short period of time.

A volvulus is when a loop of intestine twists around itself and the mesentery that supports it, resulting in a bowel obstruction. Symptoms include abdominal pain, abdominal bloating, vomiting, constipation, and bloody stool. Onset of symptoms may be rapid or more gradual. The mesentery may become so tightly twisted that blood flow to part of the intestine is cut off, resulting in ischemic bowel. In this situation there may be fever or significant pain when the abdomen is touched.
A fecal impaction or an impacted bowel is a solid, immobile bulk of feces that can develop in the rectum as a result of chronic constipation. Fecal impaction is a common result of neurogenic bowel dysfunction and causes immense discomfort and pain. Its treatment includes laxatives, enemas, and pulsed irrigation evacuation (PIE) as well as digital removal. It is not a condition that resolves without direct treatment.
Intestinal malrotation is a congenital anomaly of rotation of the midgut. It occurs during the first trimester as the fetal gut undergoes a complex series of growth and development. Malrotation can lead to a dangerous complication called volvulus, in which cases emergency surgery is indicated. Malrotation can refer to a spectrum of abnormal intestinal positioning, often including:

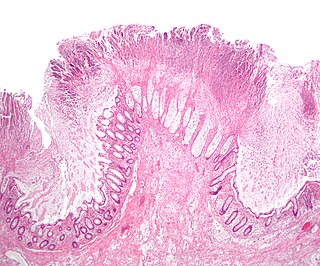
Megacolon is an abnormal dilation of the colon. This leads to hypertrophy of the colon. The dilation is often accompanied by a paralysis of the peristaltic movements of the bowel. In more extreme cases, the feces consolidate into hard masses inside the colon, called fecalomas, which can require surgery to be removed.

Intestinal pseudo-obstruction (IPO) is a clinical syndrome caused by severe impairment in the ability of the intestines to push food through. It is characterized by the signs and symptoms of intestinal obstruction without any lesion in the intestinal lumen. Clinical features mimic those seen with mechanical intestinal obstructions and can include abdominal pain, nausea, abdominal distension, vomiting, dysphagia and constipation depending upon the part of the gastrointestinal tract involved.

Ischemic colitis is a medical condition in which inflammation and injury of the large intestine result from inadequate blood supply. Although uncommon in the general population, ischemic colitis occurs with greater frequency in the elderly, and is the most common form of bowel ischemia. Causes of the reduced blood flow can include changes in the systemic circulation or local factors such as constriction of blood vessels or a blood clot. In most cases, no specific cause can be identified.

Distal intestinal obstruction syndrome (DIOS) involves obstruction of the distal part of the small intestines by thickened intestinal content and occurs in about 20% of mainly adult individuals with cystic fibrosis. DIOS was previously known as meconium ileus equivalent, a name which highlights its similarity to the intestinal obstruction seen in newborn infants with cystic fibrosis. DIOS tends to occur in older individuals with pancreatic insufficiency. Individuals with DIOS may be predisposed to bowel obstruction, though it is a separate entity than true constipation.

Chronic intestinal pseudo-obstruction (CIPO) is an uncommon syndrome with chronic and recurrent symptoms that suggest intestinal obstruction in the absence of any mechanical blockage of the lumen. The most common symptoms of CIPO include abdominal pain, constipation, nausea, vomiting, dysphagia, and abdominal distention. CIPO can lead to malnutrition.
Stercoral ulcer is an ulcer of the colon due to pressure and irritation resulting from severe, prolonged constipation due to a large bowel obstruction, damage to the autonomic nervous system, or stercoral colitis. It is most commonly located in the sigmoid colon and rectum. Prolonged constipation leads to production of fecaliths, leading to possible progression into a fecaloma. These hard lumps irritate the rectum and lead to the formation of these ulcers. It results in fresh bleeding per rectum. These ulcers may be seen on imaging, such as a CT scan but are more commonly identified using endoscopy, usually a colonoscopy. Treatment modalities can include both surgical and non-surgical techniques.

Intestinal ischemia is a medical condition in which injury to the large or small intestine occurs due to not enough blood supply. It can come on suddenly, known as acute intestinal ischemia, or gradually, known as chronic intestinal ischemia. The acute form of the disease often presents with sudden severe abdominal pain and is associated with a high risk of death. The chronic form typically presents more gradually with abdominal pain after eating, unintentional weight loss, vomiting, and fear of eating.

Prucalopride, sold under brand names Resolor and Motegrity among others, is a medication acting as a selective, high affinity 5-HT4 receptor agonist which targets the impaired motility associated with chronic constipation, thus normalizing bowel movements. Prucalopride was approved for medical use in the European Union in 2009, in Canada in 2011, in Israel in 2014, and in the United States in December 2018. The drug has also been tested for the treatment of chronic intestinal pseudo-obstruction.
Megaduodenum is a congenital or acquired dilation and elongation of the duodenum with hypertrophy of all layers that presents as a feeling of gastric fullness, abdominal pain, belching, heartburn, and nausea with vomiting sometimes of food eaten 24 hours prior.