Myoclonus is a brief, involuntary, irregular twitching of a muscle, a joint, or a group of muscles, different from clonus, which is rhythmic or regular. Myoclonus describes a medical sign and, generally, is not a diagnosis of a disease. It belongs to the hyperkinetic movement disorders, among tremor and chorea for example. These myoclonic twitches, jerks, or seizures are usually caused by sudden muscle contractions or brief lapses of contraction. The most common circumstance under which they occur is while falling asleep. Myoclonic jerks occur in healthy people and are experienced occasionally by everyone. However, when they appear with more persistence and become more widespread they can be a sign of various neurological disorders. Hiccups are a kind of myoclonic jerk specifically affecting the diaphragm. When a spasm is caused by another person it is known as a provoked spasm. Shuddering attacks in babies fall in this category.

Lennox–Gastaut syndrome (LGS) is a complex, rare, and severe childhood-onset epilepsy syndrome. It is characterized by multiple and concurrent seizure types including tonic seizure, cognitive dysfunction, and slow spike waves on electroencephalogram (EEG), which are very abnormal. Typically, it presents in children aged 3–5 years and most of the time persists into adulthood with slight changes in the electroclinical phenotype. It has been associated with perinatal injuries, congenital infections, brain malformations, brain tumors, genetic disorders such as tuberous sclerosis and numerous gene mutations. Sometimes LGS is observed after infantile epileptic spasm syndrome. The prognosis for LGS is marked by a 5% mortality in childhood and persistent seizures into adulthood.
Myoclonic epilepsy refers to a family of epilepsies that present with myoclonus. When myoclonic jerks are occasionally associated with abnormal brain wave activity, it can be categorized as myoclonic seizure. If the abnormal brain wave activity is persistent and results from ongoing seizures, then a diagnosis of myoclonic epilepsy may be considered.
Epileptic spasms is an uncommon-to-rare epileptic disorder in infants, children and adults. One of the other names of the disorder, West syndrome, is in memory of the English physician, William James West (1793–1848), who first described it in an article published in The Lancet in 1841. The original case actually described his own son, James Edwin West (1840–1860). Other names for it are "generalized flexion epilepsy", "infantile epileptic encephalopathy", "infantile myoclonic encephalopathy", "jackknife convulsions", "massive myoclonia" and "Salaam spasms". The term "infantile spasms" can be used to describe the specific seizure manifestation in the syndrome, but is also used as a synonym for the syndrome itself. West syndrome in modern usage is the triad of infantile spasms, a pathognomonic EEG pattern, and developmental regression – although the international definition requires only two out of these three elements.
In the field of neurology, seizure types are categories of seizures defined by seizure behavior, symptoms, and diagnostic tests. The International League Against Epilepsy (ILAE) 2017 classification of seizures is the internationally recognized standard for identifying seizure types. The ILAE 2017 classification of seizures is a revision of the prior ILAE 1981 classification of seizures. Distinguishing between seizure types is important since different types of seizures may have different causes, outcomes, and treatments.

Generalized epilepsy is a form of epilepsy characterised by generalised seizures with no apparent cause. Generalized seizures, as opposed to focal seizures, are a type of seizure that impairs consciousness and distorts the electrical activity of the whole or a larger portion of the brain.
Progressive Myoclonic Epilepsies (PME) are a rare group of inherited neurodegenerative diseases characterized by myoclonus, resistance to treatment, and neurological deterioration. The cause of PME depends largely on the type of PME. Most PMEs are caused by autosomal dominant or recessive and mitochondrial mutations. The location of the mutation also affects the inheritance and treatment of PME. Diagnosing PME is difficult due to their genetic heterogeneity and the lack of a genetic mutation identified in some patients. The prognosis depends largely on the worsening symptoms and failure to respond to treatment. There is no current cure for PME and treatment focuses on managing myoclonus and seizures through antiepileptic medication (AED).

Syntaxin-binding protein 1 is a protein that in humans is encoded by the STXBP1 gene. This gene encodes a syntaxin-binding protein. The encoded protein appears to play a role in release of neurotransmitters via regulation of syntaxin, a transmembrane attachment protein receptor. Mutations in this gene have been associated with neurological disorders including epilepsy, intellectual disability, and movement disorders.

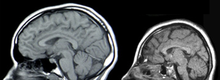
Spike-and-wave is a pattern of the electroencephalogram (EEG) typically observed during epileptic seizures. A spike-and-wave discharge is a regular, symmetrical, generalized EEG pattern seen particularly during absence epilepsy, also known as ‘petit mal’ epilepsy. The basic mechanisms underlying these patterns are complex and involve part of the cerebral cortex, the thalamocortical network, and intrinsic neuronal mechanisms.
Myoclonic astatic epilepsy (MAE), also known as myoclonic atonic epilepsy or Doose syndrome, and renamed "Epilepsy with myoclonic-atonic seizures" in the ILAE 2017 classification, is a generalized idiopathic epilepsy. It is characterized by the development of myoclonic seizures and/or myoclonic astatic seizures. Some of the common monogenic causes include mutations in the genes SLC6A1 (3p25.3),CHD2 (15q26.1), AP2M1 (10q23.2).
Jeavons syndrome is a type of epilepsy. It is one of the most distinctive reflex syndromes of idiopathic generalized epilepsy characterized by the triad of eyelid myoclonia with and without absences, eye-closure-induced seizures, EEG paroxysms, or both, and photosensitivity. Eyelid myoclonia with or without absences is a form of epileptic seizure manifesting with myoclonic jerks of the eyelids with or without a brief absence. These are mainly precipitated by closing of the eyes and lights. Eyelid myoclonia is the defining seizure type of Jeavons syndrome.
Epilepsy-intellectual disability in females also known as PCDH19 gene-related epilepsy or epileptic encephalopathy, early infantile, 9 (EIEE9), is a rare type of epilepsy that affects predominately females and is characterized by clusters of brief seizures, which start in infancy or early childhood, and is occasionally accompanied by varying degrees of cognitive impairment. The striking pattern of onset seizures at a young age, genetic testing and laboratory results, potential developmental delays or developmental regression and associated disorders, eases diagnosis.
Early myoclonic encephalopathy (EME) is a rare neonatal-onset epilepsy developmental and epileptic encephalopathy (DEE) with an onset at neonatal period or during the first 3 months of life. This syndrome is now included as part of the Early infantile developmental and epileptic encephalopathy (EIDEE) under the 2022 ILAE syndrome classification.
An epilepsy syndrome is defined as "a characteristic cluster of clinical and EEG features, often supported by specific etiological findings ."
A neonatal seizure is a seizure in a baby younger than age 4-weeks that is identifiable by an electrical recording of the brain. It is an occurrence of abnormal, paroxysmal, and persistent ictal rhythm with an amplitude of 2 microvolts in the electroencephalogram,. These may be manifested in form of stiffening or jerking of limbs or trunk. Sometimes random eye movements, cycling movements of legs, tonic eyeball movements, and lip-smacking movements may be observed. Alteration in heart rate, blood pressure, respiration, salivation, pupillary dilation, and other associated paroxysmal changes in the autonomic nervous system of infants may be caused due to these seizures. Often these changes are observed along with the observance of other clinical symptoms. A neonatal seizure may or may not be epileptic. Some of them may be provoked. Most neonatal seizures are due to secondary causes. With hypoxic ischemic encephalopathy being the most common cause in full term infants and intraventricular hemorrhage as the most common cause in preterm infants.

Solute carrier family 25 member 22 is a protein that in humans is encoded by the SLC25A22 gene. This gene encodes a mitochondrial glutamate carrier. Mutations in this gene are associated with early infantile epileptic encephalopathy. Expression of this gene is increased in colorectal tumor cells.
Barakat-Perenthaler syndrome is a rare neurodevelopmental genetic disorder, presenting with a severe epileptic encephalopathy, developmental delay, Intellectual disability, progressive microcephaly and visual disturbance. It is listed by the standard reference, Online Mendelian Inheritance in Man (OMIM) as #618744. and classified as EPILEPTIC ENCEPHALOPATHY, EARLY INFANTILE, 83; EIEE83. It was first described in 2019 by Dr. Stefan Barakat and his team at the Erasmus University Medical Center in Rotterdam in the journal Acta Neuropathologica; the most recent reviews were published in Epilepsy Currents. and Trends in Endocrinology and Metabolism
Malignant migrating partial seizures of infancy (MMPSI) is a rare epileptic syndrome that onsets before 6 months of age, commonly in the first few weeks of life. Once seizures start, the site of seizure activity repeatedly migrates from one area of the brain to another, with few periods of remission in between. These seizures are 'focal' (updated term for 'partial'), meaning they do not affect both sides of the brain at the same time. These continuous seizures cause damage to the brain, hence the descriptor 'malignant.'
PRICKLE1-related progressive myoclonus epilepsy with ataxia is a very rare genetic disorder which is characterized by myoclonic epilepsy and ataxia.
SLC13A5 citrate transporter disorder, or SLC13A5 Epilepsy, is a rare genetic spectrum disorder that presents with neurological symptoms. Symptoms include severe seizures, ataxia, dystonia, teeth hypoplasia, poor communication skills, difficulty standing or walking, as well as developmental delay. Other names associated with SLC13A5 Epilepsy include SLC13A5 Citrate Transporter Disorder, Citrate Transporter Disorder, SLC13A5 Deficiency, Early Infantile Epilepsy Encephalopathy 25 (EIEE25), Developmental Epilepsy Encephalopathy 25 (DEE25), and Kohlschutter-Tonz Syndrome (non-ROGDI).