Decompression sickness is a medical condition caused by dissolved gases emerging from solution as bubbles inside the body tissues during decompression. DCS most commonly occurs during or soon after a decompression ascent from underwater diving, but can also result from other causes of depressurisation, such as emerging from a caisson, decompression from saturation, flying in an unpressurised aircraft at high altitude, and extravehicular activity from spacecraft. DCS and arterial gas embolism are collectively referred to as decompression illness.

Hypothermia is defined as a body core temperature below 35.0 °C (95.0 °F) in humans. Symptoms depend on the temperature. In mild hypothermia, there is shivering and mental confusion. In moderate hypothermia, shivering stops and confusion increases. In severe hypothermia, there may be hallucinations and paradoxical undressing, in which a person removes their clothing, as well as an increased risk of the heart stopping.

Gangrene is a type of tissue death caused by a lack of blood supply. Symptoms may include a change in skin color to red or black, numbness, swelling, pain, skin breakdown, and coolness. The feet and hands are most commonly affected. If the gangrene is caused by an infectious agent, it may present with a fever or sepsis.

A blister is a small pocket of body fluid within the upper layers of the skin, usually caused by forceful rubbing (friction), burning, freezing, chemical exposure or infection. Most blisters are filled with a clear fluid, either serum or plasma. However, blisters can be filled with blood or with pus.

Necrotizing fasciitis (NF), also known as flesh-eating disease, is a bacterial infection that results in the death of parts of the body's soft tissue. It is a severe disease of sudden onset that spreads rapidly. Symptoms usually include red or purple skin in the affected area, severe pain, fever, and vomiting. The most commonly affected areas are the limbs and perineum.

Barotrauma is physical damage to body tissues caused by a difference in pressure between a gas space inside, or in contact with, the body and the surrounding gas or liquid. The initial damage is usually due to over-stretching the tissues in tension or shear, either directly by an expansion of the gas in the closed space or by pressure difference hydrostatically transmitted through the tissue. Tissue rupture may be complicated by the introduction of gas into the local tissue or circulation through the initial trauma site, which can cause blockage of circulation at distant sites or interfere with the normal function of an organ by its presence. The term is usually applied when the gas volume involved already exists prior to decompression. Barotrama can occur during both compression and decompression events.

Ischemia or ischaemia is a restriction in blood supply to any tissue, muscle group, or organ of the body, causing a shortage of oxygen that is needed for cellular metabolism. Ischemia is generally caused by problems with blood vessels, with resultant damage to or dysfunction of tissue i.e. hypoxia and microvascular dysfunction. It also implies local hypoxia in a part of a body resulting from constriction.

Chilblains, also known as pernio, is a medical condition in which damage occurs to capillary beds in the skin, most often in the hands or feet, when blood perfuses into the nearby tissue, resulting in redness, itching, inflammation, and possibly blisters.
Cryotherapy, sometimes known as cold therapy, is the local or general use of low temperatures in medical therapy. Cryotherapy may be used to treat a variety of tissue lesions. The most prominent use of the term refers to the surgical treatment, specifically known as cryosurgery or cryoablation. Cryosurgery is the application of extremely low temperatures to destroy abnormal or diseased tissue and is used most commonly to treat skin conditions.

CREST syndrome, also known as the limited cutaneous form of systemic sclerosis (lcSSc), is a multisystem connective tissue disorder. The acronym "CREST" refers to the five main features: calcinosis, Raynaud's phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia.
Diving disorders, or diving related medical conditions, are conditions associated with underwater diving, and include both conditions unique to underwater diving, and those that also occur during other activities. This second group further divides into conditions caused by exposure to ambient pressures significantly different from surface atmospheric pressure, and a range of conditions caused by general environment and equipment associated with diving activities.

Iloprost, sold under the brand name Ventavis among others, is a medication used to treat pulmonary arterial hypertension (PAH), scleroderma, Raynaud's phenomenon, frostbite, and other conditions in which the blood vessels are constricted and blood cannot flow to the tissues. Iloprost is a prostacyclin mimetic.
Ebullism is the formation of water vapour bubbles in bodily fluids due to reduced environmental pressure, usually at extreme high altitude. It occurs because a system of liquid and gas at equilibrium will see a net conversion of liquid to gas as pressure lowers; for example, liquids reach their boiling points at lower temperatures when the pressure on them is lowered. The injuries and disorder caused by ebullism is also known as ebullism syndrome. Ebullism will expand the volume of the tissues, but the vapour pressure of water at temperatures in which a human can survive is not sufficient to rupture skin or most other tissues encased in skin. Ebullism produces predictable injuries, which may be survivable if treated soon enough, and is often accompanied by complications caused by rapid decompression, such as decompression sickness and a variety of barotrauma injuries. Persons at risk are astronauts and high altitude aviators, for whom it is an occupational hazard.
Deep hypothermic circulatory arrest (DHCA) is a surgical technique in which the temperature of the body falls significantly and blood circulation is stopped for up to one hour. It is used when blood circulation to the brain must be stopped because of delicate surgery within the brain, or because of surgery on large blood vessels that lead to or from the brain. DHCA is used to provide a better visual field during surgery due to the cessation of blood flow. DHCA is a form of carefully managed clinical death in which heartbeat and all brain activity cease.
Cold compression therapy, also known as hilotherapy, combines two of the principles of rest, ice, compression, elevation to reduce pain and swelling from a sports or activity injury to soft tissues and is recommended by orthopedic surgeons following surgery. The therapy is especially useful for sprains, strains, pulled muscles and pulled ligaments.

Trench foot, also known by other names, is a type of foot damage due to moisture. Initial symptoms often include tingling or itching which can progress to numbness. The feet may become red or bluish in color. As the condition worsens the feet can start to swell and smell of decay. Complications may include skin breakdown or infection.

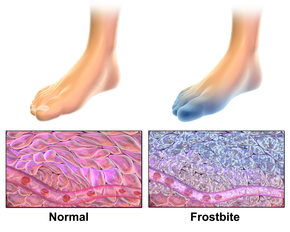
Cold injury is damage to the body from cold exposure, including hypothermia and several skin injuries. Cold-related skin injuries are categorized into freezing and nonfreezing cold injuries. Freezing cold injuries involve tissue damage when exposed to temperatures below freezing. Nonfreezing cold injuries involve tissue damage when exposed to temperatures often between 0-15 degrees Celsius for extended periods of time. While these injuries have disproportionally affected military members, recreational winter activities have also increased the risk and incidence within civilian populations. Additional risk factors include homelessness, inadequate or wet clothing, alcohol abuse or tobacco abuse, and pre-existing medical conditions that impair blood flow.

An aerosol frostbite of the skin is an injury to the body caused by the pressurized gas within an aerosol spray cooling quickly, with the sudden drop in temperature sufficient to cause frostbite to the applied area. Medical studies have noted an increase of this practice, known as "frosting", in pediatric and teenage patients.
Non-freezing cold injuries (NFCI) is a class of tissue damage caused by sustained exposure to low temperature without actual freezing. There are several forms of NFCI, and the common names may refer to the circumstances in which they commonly occur or were first described, such as trench foot, which was named after its association with trench warfare. NFCI is caused by microvascular endothelial damage, stasis and vascular occlusion and is characterised by peripheral neuropathy. NFCI generally affects the hands or feet during exposure to temperatures just above freezing, often wet, and is typically found in soldiers.
Inner ear decompression sickness, (IEDCS) or audiovestibular decompression sickness is a medical condition of the inner ear caused by the formation of gas bubbles in the tissues or blood vessels of the inner ear. Generally referred to as a form of decompression sickness, it can also occur at constant pressure due to inert gas counterdiffusion effects.