Related Research Articles
An anxiolytic is a medication or other intervention that reduces anxiety. This effect is in contrast to anxiogenic agents which increase anxiety. Anxiolytic medications are used for the treatment of anxiety disorders and their related psychological and physical symptoms.
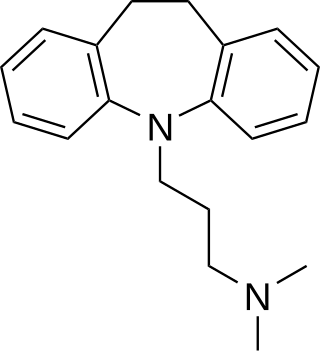
Tricyclic antidepressants (TCAs) are a class of medications that are used primarily as antidepressants. TCAs were discovered in the early 1950s and were marketed later in the decade. They are named after their chemical structure, which contains three rings of atoms. Tetracyclic antidepressants (TeCAs), which contain four rings of atoms, are a closely related group of antidepressant compounds.

Psychopharmacology is the scientific study of the effects drugs have on mood, sensation, thinking, behavior, judgment and evaluation, and memory. It is distinguished from neuropsychopharmacology, which emphasizes the correlation between drug-induced changes in the functioning of cells in the nervous system and changes in consciousness and behavior.
A psychiatric or psychotropic medication is a psychoactive drug taken to exert an effect on the chemical makeup of the brain and nervous system. Thus, these medications are used to treat mental illnesses. These medications are typically made of synthetic chemical compounds and are usually prescribed in psychiatric settings, potentially involuntarily during commitment. Since the mid-20th century, such medications have been leading treatments for a broad range of mental disorders and have decreased the need for long-term hospitalization, thereby lowering the cost of mental health care. The recidivism or rehospitalization of the mentally ill is at a high rate in many countries, and the reasons for the relapses are under research.

The atypical antipsychotics (AAP), also known as second generation antipsychotics (SGAs) and serotonin–dopamine antagonists (SDAs), are a group of antipsychotic drugs largely introduced after the 1970s and used to treat psychiatric conditions. Some atypical antipsychotics have received regulatory approval for schizophrenia, bipolar disorder, irritability in autism, and as an adjunct in major depressive disorder.

Tetracyclic antidepressants (TeCAs) are a class of antidepressants that were first introduced in the 1970s. They are named after their tetracyclic chemical structure, containing four rings of atoms, and are closely related to the tricyclic antidepressants (TCAs), which contain three rings of atoms.

Azapirones are a class of drugs used as anxiolytics, antidepressants, and antipsychotics. They are commonly used as add-ons to other antidepressants, such as selective serotonin reuptake inhibitors (SSRIs).

Amoxapine, sold under the brand name Asendin among others, is a tricyclic antidepressant (TCA). It is the N-demethylated metabolite of loxapine. Amoxapine first received marketing approval in the United States in 1980, approximately 10 to 20 years after most of the other TCAs were introduced in the United States.

Noradrenergic and specific serotonergic antidepressants (NaSSAs) are a class of psychiatric drugs used primarily as antidepressants. They act by antagonizing the α2-adrenergic receptor and certain serotonin receptors such as 5-HT2A and 5-HT2C, but also 5-HT3, 5-HT6, and/or 5-HT7 in some cases. By blocking α2-adrenergic autoreceptors and heteroreceptors, NaSSAs enhance adrenergic and serotonergic neurotransmission in the brain involved in mood regulation, notably 5-HT1A-mediated transmission. In addition, due to their blockade of certain serotonin receptors, serotonergic neurotransmission is not facilitated in unwanted areas, which prevents the incidence of many side effects often associated with selective serotonin reuptake inhibitor (SSRI) antidepressants; hence, in part, the "specific serotonergic" label of NaSSAs.

Trimipramine, sold under the brand name Surmontil among others, is a tricyclic antidepressant (TCA) which is used to treat depression. It has also been used for its sedative, anxiolytic, and weak antipsychotic effects in the treatment of insomnia, anxiety disorders, and psychosis, respectively. The drug is described as an atypical or "second-generation" TCA because, unlike other TCAs, it seems to be a fairly weak monoamine reuptake inhibitor. Similarly to other TCAs, however, trimipramine does have antihistamine, antiserotonergic, antiadrenergic, antidopaminergic, and anticholinergic activities.
A serotonin–norepinephrine–dopamine reuptake inhibitor (SNDRI), also known as a triple reuptake inhibitor (TRI), is a type of drug that acts as a combined reuptake inhibitor of the monoamine neurotransmitters serotonin, norepinephrine, and dopamine. It does this by concomitantly inhibiting the serotonin transporter (SERT), norepinephrine transporter (NET), and dopamine transporter (DAT), respectively. Inhibition of the reuptake of these neurotransmitters increases their extracellular concentrations and, therefore, results in an increase in serotonergic, adrenergic, and dopaminergic neurotransmission. The naturally-occurring and potent SNDRI cocaine is widely used recreationally and often illegally for the euphoric effects it produces.

A serotonin reuptake inhibitor (SRI) is a type of drug which acts as a reuptake inhibitor of the neurotransmitter serotonin by blocking the action of the serotonin transporter (SERT). This in turn leads to increased extracellular concentrations of serotonin and, therefore, an increase in serotonergic neurotransmission. It is a type of monoamine reuptake inhibitor (MRI); other types of MRIs include dopamine reuptake inhibitors and norepinephrine reuptake inhibitors.

A norepinephrine and dopamine disinhibitor is a drug that acts at specific sites to disinhibit downstream norepinephrine and dopamine release in the brain.

Metapramine is a tricyclic antidepressant (TCA) developed by Rhone Poulenc that was introduced for the treatment of depression in France in 1984. In addition to its efficacy against affective disorders, it also has analgesic properties, and may be useful in the treatment of pain.
The pharmacology of antidepressants is not entirely clear. The earliest and probably most widely accepted scientific theory of antidepressant action is the monoamine hypothesis, which states that depression is due to an imbalance of the monoamine neurotransmitters. It was originally proposed based on the observation that certain hydrazine anti-tuberculosis agents produce antidepressant effects, which was later linked to their inhibitory effects on monoamine oxidase, the enzyme that catalyses the breakdown of the monoamine neurotransmitters. All currently marketed antidepressants have the monoamine hypothesis as their theoretical basis, with the possible exception of agomelatine which acts on a dual melatonergic-serotonergic pathway. Despite the success of the monoamine hypothesis it has a number of limitations: for one, all monoaminergic antidepressants have a delayed onset of action of at least a week; and secondly, there are a sizeable portion (>40%) of depressed patients that do not adequately respond to monoaminergic antidepressants. Further evidence to the contrary of the monoamine hypothesis are the recent findings that a single intravenous infusion with ketamine, an antagonist of the NMDA receptor — a type of glutamate receptor — produces rapid, robust and sustained antidepressant effects. Monoamine precursor depletion also fails to alter mood. To overcome these flaws with the monoamine hypothesis a number of alternative hypotheses have been proposed, including the glutamate, neurogenic, epigenetic, cortisol hypersecretion and inflammatory hypotheses. Another hypothesis that has been proposed which would explain the delay is the hypothesis that monoamines don't directly influence mood, but influence emotional perception biases.
A serotonin modulator and stimulator (SMS), sometimes referred to more simply as a serotonin modulator, is a type of drug with a multimodal action specific to the serotonin neurotransmitter system. To be precise, SMSs simultaneously modulate one or more serotonin receptors and inhibit the reuptake of serotonin. The term was created to describe the mechanism of action of the serotonergic antidepressant vortioxetine, which acts as a serotonin reuptake inhibitor (SRI), agonist of the 5-HT1A receptor, and antagonist of the 5-HT3 and 5-HT7 receptors. However, it can also technically be applied to vilazodone, which is an antidepressant as well and acts as an SRI and 5-HT1A receptor partial agonist.
The conditioned avoidance response (CAR) test, also known as the active avoidance test, is an animal test used to identify drugs with antipsychotic-like effects. It is most commonly employed as a two-way active avoidance test with rodents. The test assesses the conditioned ability of an animal to avoid an unpleasant stimulus. Drugs that selectively suppress conditioned avoidance responses without affecting escape behavior are considered to have antipsychotic-like activity. Variations of the test, like testing for enhancement of avoidance and escape responses, have also been used to assess other drug effects, like pro-motivational and antidepressant-like effects.
References
- ↑ Tatsumi M, Groshan K, Blakely RD, Richelson E (December 1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters". European Journal of Pharmacology. 340 (2–3): 249–258. doi:10.1016/s0014-2999(97)01393-9. PMID 9537821.
- ↑ Fedder D, Patel H, Saadabadi A (March 2023). "Atomoxetine". StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. PMID 29630286.
- ↑ Dell'Osso B, Palazzo MC, Oldani L, Altamura AC (December 2011). "The noradrenergic action in antidepressant treatments: pharmacological and clinical aspects". CNS Neurosci Ther. 17 (6): 723–32. doi:10.1111/j.1755-5949.2010.00217.x. PMC 6493872 . PMID 21155988.
- ↑ Fleurence R, Williamson R, Jing Y, Kim E, Tran QV, Pikalov AS, et al. (2009). "A systematic review of augmentation strategies for patients with major depressive disorder". Psychopharmacol Bull. 42 (3): 57–90. PMID 19752841.
- 1 2 Corp SA, Gitlin MJ, Altshuler LL (September 2014). "A review of the use of stimulants and stimulant alternatives in treating bipolar depression and major depressive disorder". J Clin Psychiatry. 75 (9): 1010–8. doi:10.4088/JCP.13r08851. PMID 25295426.
- ↑ Arias HR, Santamaría A, Ali SF (2009). "Pharmacological and neurotoxicological actions mediated by bupropion and diethylpropion". Int. Rev. Neurobiol. International Review of Neurobiology. 88: 223–55. doi:10.1016/S0074-7742(09)88009-4. ISBN 9780123745040. PMID 19897080.
- ↑ Dale E, Bang-Andersen B, Sánchez C (2015). "Emerging mechanisms and treatments for depression beyond SSRIs and SNRIs". Biochem. Pharmacol. 95 (2): 81–97. doi: 10.1016/j.bcp.2015.03.011 . PMID 25813654.
- ↑ Challman TD, Lipsky JJ (2000). "Methylphenidate: its pharmacology and uses". Mayo Clin. Proc. 75 (7): 711–21. doi: 10.4065/75.7.711 . PMID 10907387.
- ↑ Prommer E (2012). "Methylphenidate: established and expanding roles in symptom management". Am J Hosp Palliat Care. 29 (6): 483–90. doi:10.1177/1049909111427029. PMID 22144657. S2CID 21384037.
- ↑ Urban AE, Cubała WJ (February 2020). "The role of eugeroics in the treatment of affective disorders". Psychiatr Pol. 54 (1): 21–33. doi: 10.12740/PP/OnlineFirst/90687 . PMID 32447354.
- ↑ Kleeblatt J, Betzler F, Kilarski LL, Bschor T, Köhler S (May 2017). "Efficacy of off-label augmentation in unipolar depression: A systematic review of the evidence". Eur Neuropsychopharmacol. 27 (5): 423–441. doi:10.1016/j.euroneuro.2017.03.003. PMID 28318897. S2CID 3740987.
- ↑ Nunez NA, Singh B, Romo-Nava F, Joseph B, Veldic M, Cuellar-Barboza A, et al. (March 2020). "Efficacy and tolerability of adjunctive modafinil/armodafinil in bipolar depression: A meta-analysis of randomized controlled trials". Bipolar Disord. 22 (2): 109–120. doi: 10.1111/bdi.12859 . PMID 31643130.
- ↑ Szmulewicz AG, Angriman F, Samamé C, Ferraris A, Vigo D, Strejilevich SA (June 2017). "Dopaminergic agents in the treatment of bipolar depression: a systematic review and meta-analysis". Acta Psychiatr Scand. 135 (6): 527–538. doi:10.1111/acps.12712. PMID 28256707. S2CID 3712257.
- ↑ "SPRAVATO™ (esketamine) nasal spray FDA label" (PDF). Food and Drug Administration. 5 March 2019. Retrieved 6 March 2019.
- ↑ Zhang MW, Harris KM, Ho RC (2016). "Is off-label repeat prescription of ketamine as a rapid antidepressant safe? Controversies, ethical concerns, and legal implications". BMC Med Ethics. 17: 4. doi: 10.1186/s12910-016-0087-3 . PMC 4714497 . PMID 26768892.
- ↑ Thase ME (2016). "Adverse Effects of Second-Generation Antipsychotics as Adjuncts to Antidepressants: Are the Risks Worth the Benefits?". Psychiatr. Clin. North Am. 39 (3): 477–86. doi:10.1016/j.psc.2016.04.008. PMID 27514300.