In published academic research, publication bias occurs when the outcome of an experiment or research study biases the decision to publish or otherwise distribute it. Publishing only results that show a significant finding disturbs the balance of findings in favor of positive results. The study of publication bias is an important topic in metascience.
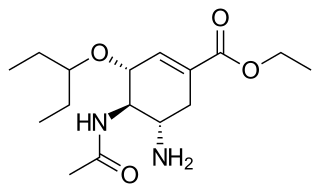
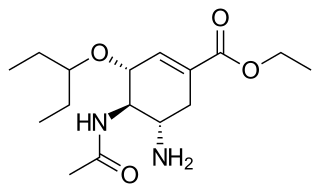
Oseltamivir, sold under the brand name Tamiflu, is an antiviral medication used to treat and prevent influenza A and influenza B, viruses that cause the flu. Many medical organizations recommend it in people who have complications or are at high risk of complications within 48 hours of first symptoms of infection. They recommend it to prevent infection in those at high risk, but not the general population. The Centers for Disease Control and Prevention (CDC) recommends that clinicians use their discretion to treat those at lower risk who present within 48 hours of first symptoms of infection. It is taken by mouth, either as a pill or liquid.
Male circumcision reduces the risk of human immunodeficiency virus (HIV) transmission from HIV positive women to men in high risk populations.

Joseph Marie Albert "Joep" Lange was a Dutch clinical researcher specialising in HIV therapy. He served as the president of the International AIDS Society from 2002 to 2004. He was a passenger on Malaysia Airlines Flight 17, which was shot down on 17 July 2014 over Ukraine.

Circumcision is a procedure that removes the foreskin from the human penis. In the most common form of the operation, the foreskin is extended with forceps, then a circumcision device may be placed, after which the foreskin is excised. Topical or locally injected anesthesia is generally used to reduce pain and physiologic stress. Circumcision is generally electively performed, most commonly done as a form of preventive healthcare, as a religious obligation, or as a cultural practice. It is also an option for cases of phimosis, other pathologies that do not resolve with other treatments, and chronic urinary tract infections (UTIs). The procedure is contraindicated in cases of certain genital structure abnormalities or poor general health.
The STROBE(STrengthening the Reporting of OBservational studies in Epidemiology) Statement is a reporting guideline including a checklist of 22 items that are considered essential for good reporting of observational studies. It was published simultaneously in several leading biomedical journals in October and November 2007 and comprises both the checklist and an explanation and elaboration article which gives examples of good reporting and provides authors with more guidance on good reporting. It is also referred to in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals established by the International Committee of Medical Journal Editors and is endorsed by hundreds of biomedical journals.
Peter Christian Gøtzsche is a Danish physician, medical researcher, and former leader of the Nordic Cochrane Center at Rigshospitalet in Copenhagen, Denmark. He is a co-founder of the Cochrane Collaboration and has written numerous reviews for the organization. His membership in Cochrane was terminated by its Governing Board of Trustees on 25 September 2018.

John P. A. Ioannidis is a Greek-American physician-scientist, writer and Stanford University professor who has made contributions to evidence-based medicine, epidemiology, and clinical research. Ioannidis studies scientific research itself, meta-research primarily in clinical medicine and the social sciences.

Irving Kirsch is an American psychologist and academic. He is the Associate Director of the Program in Placebo Studies and a lecturer in medicine at the Harvard Medical School and Beth Israel Deaconess Medical Center. He is also professor emeritus of psychology at the Universities of Hull and Plymouth in the United Kingdom, and the University of Connecticut in the United States. Kirsch is a leading researcher within the field of placebo studies who is noted for his work on placebo effects, antidepressants, expectancy, and hypnosis. He is the originator of response expectancy theory, and his analyses of clinical trials of antidepressants have influenced official treatment guidelines in the United Kingdom. He is the author of the 2009 book The Emperor's New Drugs, which argued most antidepressant medication is effective primarily due to placebo effects.

"Why Most Published Research Findings Are False" is a 2005 essay written by John Ioannidis, a professor at the Stanford School of Medicine, and published in PLOS Medicine. It is considered foundational to the field of metascience.
HIV prevention refers to practices that aim to prevent the spread of the human immunodeficiency virus (HIV). HIV prevention practices may be undertaken by individuals to protect their own health and the health of those in their community, or may be instituted by governments and community-based organizations as public health policies.
PharmedOut (PhO) is a Georgetown University Medical Center project founded in 2006. It is directed by Adriane Fugh-Berman. The stated mission of the organization is to advance evidence-based prescribing and educate healthcare professionals about pharmaceutical marketing practices.
White hat bias (WHB) is a purported "bias leading to the distortion of information in the service of what may be perceived to be righteous ends", which consist of both cherry picking the evidence and publication bias. Public health researchers David Allison and Mark Cope first discussed this bias in a 2010 paper and explained the motivation behind it in terms of "righteous zeal, indignation toward certain aspects of industry", and other factors.
Sema K. Sgaier is a scientist, global health expert, and documentary photographer. Sgaier’s expertise includes molecular biology, genetics, genomics, neuroscience, epidemiology, disease surveillance, monitoring & evaluation of programs and policy development.

PRISMA is an evidence-based minimum set of items aimed at helping scientific authors to report a wide array of systematic reviews and meta-analyses, primarily used to assess the benefits and harms of a health care intervention. PRISMA focuses on ways in which authors can ensure a transparent and complete reporting of this type of research. The PRISMA standard superseded the earlier QUOROM standard. It offers the replicability of a systematic literature review. Researchers have to figure out research objectives that answer the research question, states the keywords, a set of exclusion and inclusion criteria. In the review stage, relevant articles were searched, irrelevant ones are removed. Articles are analyzed according to some pre-defined categories.

Elioda Tumwesigye is a Ugandan politician, physician, and epidemiologist who has served as minister of science, technology and innovation in the cabinet of Uganda since June 2016. From March 2015 until June 2016, he served as the minister of health.

Jane Ruth Aceng is a Ugandan pediatrician and politician. She is the Minister of Health in the Cabinet of Uganda. She was appointed to that position on 6 June 2016. Before that, from June 2011 until June 2016, she served as the Director General of Medical Services in the Ugandan Ministry of Health.

Conflicts of interest (COIs) often arise in academic publishing. Such conflicts may cause wrongdoing and make it more likely. Ethical standards in academic publishing exist to avoid and deal with conflicts of interest, and the field continues to develop new standards. Standards vary between journals and are unevenly applied. According to the International Committee of Medical Journal Editors, "[a]uthors have a responsibility to evaluate the integrity, history, practices and reputation of the journals to which they submit manuscripts".
Roy D. Mugerwa was a Ugandan physician, cardiologist and researcher. His contribution to the world of academics include being a Professor Emeritus at Makerere University College of Health Sciences in Kampala, cardiology in Uganda, researching HIV/AIDS and tuberculosis, and his efforts to find an effective HIV vaccine.
Elizabeth Anne Bukusi FAAS is a research professor working within the field of obstetrics and gynaecology, and global health. Bukusi's main areas of research focus around sexually transmitted infections, women's health, reproductive health, and HIV care, prevention and treatment. Bukusi is the Chief Research Officer at the Kenya Medical Research Institute (KEMRI) and led a "landmark" study on the use of PrEP in Kenya.