Related Research Articles
Insulin resistance (IR) is a pathological condition in which cells either fail to respond normally to the hormone insulin or downregulate insulin receptors in response to hyperinsulinemia.

Type 2 diabetes (T2D), formerly known as adult-onset diabetes, is a form of diabetes mellitus that is characterized by high blood sugar, insulin resistance, and relative lack of insulin. Common symptoms include increased thirst, frequent urination, fatigue and unexplained weight loss. Symptoms may also include increased hunger, having a sensation of pins and needles, and sores (wounds) that do not heal. Often symptoms come on slowly. Long-term complications from high blood sugar include heart disease, strokes, diabetic retinopathy which can result in blindness, kidney failure, and poor blood flow in the limbs which may lead to amputations. The sudden onset of hyperosmolar hyperglycemic state may occur; however, ketoacidosis is uncommon.

Leptin also obese protein is a protein hormone predominantly made by adipocytes. Its primary role is likely to regulate long-term energy balance.

Appetite is the desire to eat food items, usually due to hunger. Appealing foods can stimulate appetite even when hunger is absent, although appetite can be greatly reduced by satiety. Appetite exists in all higher life-forms, and serves to regulate adequate energy intake to maintain metabolic needs. It is regulated by a close interplay between the digestive tract, adipose tissue and the brain. Appetite has a relationship with every individual's behavior. Appetitive behaviour also known as approach behaviour, and consummatory behaviour, are the only processes that involve energy intake, whereas all other behaviours affect the release of energy. When stressed, appetite levels may increase and result in an increase of food intake. Decreased desire to eat is termed anorexia, while polyphagia is increased eating. Dysregulation of appetite contributes to anorexia nervosa, bulimia nervosa, cachexia, overeating, and binge eating disorder.

The blood sugar level, blood sugar concentration, blood glucose level, or glycemia is the measure of glucose concentrated in the blood. The body tightly regulates blood glucose levels as a part of metabolic homeostasis.

Ketogenesis is the biochemical process through which organisms produce ketone bodies by breaking down fatty acids and ketogenic amino acids. The process supplies energy to certain organs, particularly the brain, heart and skeletal muscle, under specific scenarios including fasting, caloric restriction, sleep, or others.
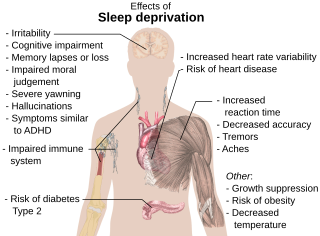
Sleep debt or sleep deficit is the cumulative effect of not getting enough sleep. A large sleep debt may lead to mental or physical fatigue, and can adversely affect one's mood, energy, and ability to think clearly.

Adiponectin is a protein hormone and adipokine, which is involved in regulating glucose levels and fatty acid breakdown. In humans, it is encoded by the ADIPOQ gene and is produced primarily in adipose tissue, but also in muscle and even in the brain.

Ghrelin is a hormone primarily produced by enteroendocrine cells of the gastrointestinal tract, especially the stomach, and is often called a "hunger hormone" because it increases the drive to eat. Blood levels of ghrelin are highest before meals when hungry, returning to lower levels after mealtimes. Ghrelin may help prepare for food intake by increasing gastric motility and stimulating the secretion of gastric acid.

Weight gain is an increase in body weight. This can involve an increase in muscle mass, fat deposits, excess fluids such as water or other factors. Weight gain can be a symptom of a serious medical condition.

Hyperinsulinemia is a condition in which there are excess levels of insulin circulating in the blood relative to the level of glucose. While it is often mistaken for diabetes or hyperglycaemia, hyperinsulinemia can result from a variety of metabolic diseases and conditions, as well as non-nutritive sugars in the diet. While hyperinsulinemia is often seen in people with early stage type 2 diabetes mellitus, it is not the cause of the condition and is only one symptom of the disease. Type 1 diabetes only occurs when pancreatic beta-cell function is impaired. Hyperinsulinemia can be seen in a variety of conditions including diabetes mellitus type 2, in neonates and in drug-induced hyperinsulinemia. It can also occur in congenital hyperinsulinism, including nesidioblastosis.

Reactive hypoglycemia, postprandial hypoglycemia, or sugar crash is a term describing recurrent episodes of symptomatic hypoglycemia occurring within four hours after a high carbohydrate meal in people with and without diabetes. The term is not necessarily a diagnosis since it requires an evaluation to determine the cause of the hypoglycemia.
Nesfatin-1 is a neuropeptide produced in the hypothalamus of mammals. It participates in the regulation of hunger and fat storage. Increased nesfatin-1 in the hypothalamus contributes to diminished hunger, a 'sense of fullness', and a potential loss of body fat and weight.

Blood sugar regulation is the process by which the levels of blood sugar, the common name for glucose dissolved in blood plasma, are maintained by the body within a narrow range.

Equine metabolic syndrome (EMS) is an endocrinopathy affecting horses and ponies. It is of primary concern due to its link to obesity, insulin dysregulation, and subsequent laminitis. There are some similarities in clinical signs between EMS and pituitary pars intermedia dysfunction, also known as PPID or Cushing's disease, and some equines may develop both, but they are not the same condition, having different causes and different treatment.
Hunger is a sensation that motivates the consumption of food. The sensation of hunger typically manifests after only a few hours without eating and is generally considered to be unpleasant. Satiety occurs between 5 and 20 minutes after eating. There are several theories about how the feeling of hunger arises. The desire to eat food, or appetite, is another sensation experienced with regard to eating.
Ingestive behaviors encompass all eating and drinking behaviors. These actions are influenced by physiological regulatory mechanisms; these mechanisms exist to control and establish homeostasis within the human body. Disruptions in these ingestive regulatory mechanisms can result in eating disorders such as obesity, anorexia, and bulimia.

The sympathoadrenal system is a physiological connection between the sympathetic nervous system and the adrenal medulla and is crucial in an organism's physiological response to outside stimuli. When the body receives sensory information, the sympathetic nervous system sends a signal to preganglionic nerve fibers, which activate the adrenal medulla through acetylcholine. Once activated, norepinephrine and epinephrine are released directly into the blood by adrenomedullary cells where they act as the bodily mechanism for "fight-or-flight" responses. Because of this, the sympathoadrenal system plays a large role in maintaining glucose levels, sodium levels, blood pressure, and various other metabolic pathways that couple with bodily responses to the environment. During numerous diseased states, such as hypoglycemia or even stress, the body's metabolic processes are skewed. The sympathoadrenal system works to return the body to homeostasis through the activation or inactivation of the adrenal gland. However, more severe disorders of the sympathoadrenal system such as pheochromocytoma can affect the body's ability to maintain a homeostatic state. In these cases, curative agents such as adrenergic agonists and antagonists are used to modify epinephrine and norepinephrine levels released by the adrenal medulla.
Sleep and weight is the association between the amount of sleep an individual obtains and the weight of that individual.

Pathophysiology of obesity is the study of disordered physiological processes that cause, result from, or are otherwise associated with obesity. A number of possible pathophysiological mechanisms have been identified which may contribute in the development and maintenance of obesity.
References
- 1 2 3 4 Sharma, Sunil; Kavuru, Mani (2 August 2010). "Sleep and Metabolism: Overview". International Journal of Endocrinology. 2010: 1–12. doi: 10.1155/2010/270832 . PMC 2929498 . PMID 20811596.
- 1 2 3 4 5 Walker, Matthew (October 10, 2011). "Sleep Deprivation I: Immune Function and Metabolism".
- 1 2 Knutson, Kristen L.; Spiegel, Karine; Penev, Plamen; Van Cauter, Eve (June 2007). "The metabolic consequences of sleep deprivation". Sleep Medicine Reviews. 11 (3): 163–178. doi:10.1016/j.smrv.2007.01.002. PMC 1991337 . PMID 17442599.
- 1 2 Darraj, Ali (2023-11-03). "The Link Between Sleeping and Type 2 Diabetes: A Systematic Review". Cureus. 15 (11): e48228. doi: 10.7759/cureus.48228 . ISSN 2168-8184. PMC 10693913 . PMID 38050514.
- 1 2 "Lack of Deep Sleep May Increase Risk of Type 2 Diabetes". Science Daily. Retrieved November 30, 2011.
- ↑ "Sleep and Metabolism: An Overview".
- ↑ "Daytime Sleepiness is associated with an increased craving for carbs among teen". Science Daily. Retrieved November 30, 2011.
- ↑ Trebekk (2007). "Sleep and metabolic control: waking to a problem?". Clinical and Experimental Pharmacology and Physiology. 34 (1–2): 2–3.
- ↑ Fatima, Y.; Doi, S. A. R.; Mamun, A. A. (2016). "Sleep quality and obesity in young subjects: a meta-analysis" (PDF). Obesity Reviews. 17 (11): 1154–1166. doi:10.1111/obr.12444. ISSN 1467-7881. PMID 27417913.
- ↑ Strobel, Richard J.; Rosen, Raymond C. (1996). "Obesity and Weight Loss in Obstructive Sleep Apnea: A Critical Review". Sleep. 19 (2): 104–115. doi:10.1093/sleep/19.2.104. ISSN 1550-9109. PMID 8855032.
- 1 2 Morrison, Matthew; Halson, Shona L.; Weakley, Jonathon; Hawley, John A. (2022-12-01). "Sleep, circadian biology and skeletal muscle interactions: Implications for metabolic health" (PDF). Sleep Medicine Reviews. 66: 101700. doi:10.1016/j.smrv.2022.101700. ISSN 1087-0792. PMID 36272396.