Neurophysiology
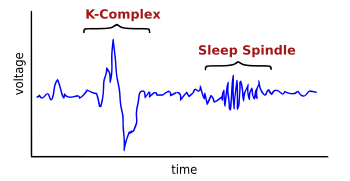
K-complex consists of a brief negative high-voltage peak, usually greater than 100 μV, followed by a slower positive complex around 350 and 550 ms and at 900 ms a final negative peak. K-complexes occur roughly every 1.0–1.7 minutes and are often followed by bursts of sleep spindles. They occur spontaneously [1] but also occur in response to external stimuli such as sounds, touches on the skin [3] and internal ones such as inspiratory interruptions. [4] They are generated in widespread cortical locations [1] though they tend to predominate over the frontal parts of the brain. [5]
Both K-complex and delta wave activity in stage 2 sleep create slow-wave (0.8 Hz) and delta (1.6–4.0 Hz) oscillations. However, their topographical distribution is different, and the delta power of K-complexes is higher. [6]
They are created by the occurrence in widespread cortical areas of outward dendritic currents from the middle (III) to the upper (I) layers of the cerebral cortex. This is accompanied by a decrease in broadband EEG power including gamma wave activity. This produces "down-states" of neuronal silence in which neural network activity is reduced. [1] The activity of K-complexes is transferred to the thalamus where it synchronizes the thalamocortical network during sleep, producing sleep oscillations such as spindles and delta waves. [7] It has been observed that they are indeed identical in the "laminar distributions of transmembrane currents" to the slow waves of slow-wave sleep. [1]
K-complexes have been suggested both to protect sleep and also to engage in information processing, as they are both an essential part of the synchronization of NREM sleep, while they also respond to both internal and external stimuli in a reactive manner. [8] This would be consistent with a function in suppressing cortical arousal in response to stimuli that the brain needs to initially process in regard to whether it is dangerous or not. [1]
Another suggested function is aiding the activation homeostasis of synapses [9] and memory consolidation. The activation thresholds of cortical synapses become lowered during wakefulness as they process information, making them more responsive, and so need to be adjusted back to preserve their signal-to-noise ratio. [9] The down-state provided by K-complexes does this by reducing the strengths of synaptic connections that occur while an individual is awake. [1] Further, the recovery from the down-state they induce allows that "cortical firing 'reboots' in a systematic order" so that memory engrams encoded during neuronal firing can be "repeatedly practiced and thus consolidated". [1]

A sleep disorder, or somnipathy, is a medical disorder of an individual's sleep patterns. Some sleep disorders are severe enough to interfere with normal physical, mental, social and emotional functioning. Sleep disorders are frequent and can have serious consequences on patients' health and quality of life. Polysomnography and actigraphy are tests commonly ordered for diagnosing sleep disorders.

Delta waves are high amplitude neural oscillations with a frequency between 0.5 and 4 hertz. Delta waves, like other brain waves, can be recorded with electroencephalography (EEG) and are usually associated with the deep stage 3 of NREM sleep, also known as slow-wave sleep (SWS), and aid in characterizing the depth of sleep. Suppression of delta waves leads to inability of body rejuvenation, brain revitalization and poor sleep.
Non-rapid eye movement sleep (NREM), also known as quiescent sleep, is, collectively, sleep stages 1–3, previously known as stages 1–4. Rapid eye movement sleep (REM) is not included. There are distinct electroencephalographic and other characteristics seen in each stage. Unlike REM sleep, there is usually little or no eye movement during these stages. Dreaming occurs during both sleep states, and muscles are not paralyzed as in REM sleep. People who do not go through the sleeping stages properly get stuck in NREM sleep, and because muscles are not paralyzed a person may be able to sleepwalk. According to studies, the mental activity that takes place during NREM sleep is believed to be thought-like, whereas REM sleep includes hallucinatory and bizarre content. NREM sleep is characteristic of dreamer-initiated friendliness, compared to REM sleep where it is more aggressive, implying that NREM is in charge of simulating friendly interactions. The mental activity that occurs in NREM and REM sleep is a result of two different mind generators, which also explains the difference in mental activity. In addition, there is a parasympathetic dominance during NREM. The reported differences between the REM and NREM activity are believed to arise from differences in the memory stages that occur during the two types of sleep.
Hypersomnia is a neurological disorder of excessive time spent sleeping or excessive sleepiness. It can have many possible causes and can cause distress and problems with functioning. In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), hypersomnolence, of which there are several subtypes, appears under sleep-wake disorders.
Sexsomnia, also known as sleep sex, is a distinct form of parasomnia, or an abnormal activity that occurs while an individual is asleep. Sexsomnia is characterized by an individual engaging in sexual acts while in non-rapid eye movement (NREM) sleep. Sexual behaviors that result from sexsomnia are not to be mistaken with normal nocturnal sexual behaviors, which do not occur during NREM sleep. Sexual behaviors that are viewed as normal during sleep and are accompanied by extensive research and documentation include nocturnal emissions, nocturnal erections, and sleep orgasms.
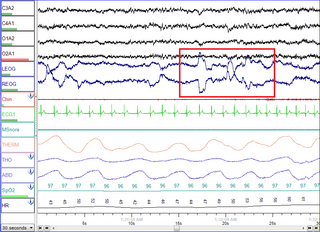
Polysomnography (PSG), a type of sleep study, is a multi-parameter study of sleep and a diagnostic tool in sleep medicine. The test result is called a polysomnogram, also abbreviated PSG. The name is derived from Greek and Latin roots: the Greek πολύς, the Latin somnus ("sleep"), and the Greek γράφειν.

The reticular formation is a set of interconnected nuclei that are located in the brainstem, hypothalamus, and other regions. It is not anatomically well defined, because it includes neurons located in different parts of the brain. The neurons of the reticular formation make up a complex set of networks in the core of the brainstem that extend from the upper part of the midbrain to the lower part of the medulla oblongata. The reticular formation includes ascending pathways to the cortex in the ascending reticular activating system (ARAS) and descending pathways to the spinal cord via the reticulospinal tracts.
The cyclic alternating pattern is a pattern of two, long-lasting alternate electroencephalogram (EEG) patterns that occur in sleep, as described by Terzano, et al., in 1985. It is a pattern of spontaneous cortical activity, which is ongoing and in the absence of sensory stimulation. It is the reorganization of the sleeping brain challenged by the modification of environmental conditions and it is characterized by periodic abnormal electrocortical activity that recurs with a frequency of up to one minute. It is considered "the EEG marker of unstable sleep". CAP does not occur during REM. In Lennox-Gastaut syndrome, CAP modulates the occurrence of clinical seizures and generalized epileptic discharges by means of a gate-control mechanism.
Periodic limb movement disorder (PLMD) is a sleep disorder where the patient moves limbs involuntarily and periodically during sleep, and has symptoms or problems related to the movement. PLMD should not be confused with restless legs syndrome (RLS), which is characterized by a voluntary response to an urge to move legs due to discomfort. PLMD on the other hand is involuntary, and the patient is often unaware of these movements altogether. Periodic limb movements (PLMs) occurring during daytime period can be found but are considered as a symptom of RLS; only PLMs during sleep can suggest a diagnosis of PLMD.
Sleep spindles are bursts of neural oscillatory activity that are generated by interplay of the thalamic reticular nucleus (TRN) and other thalamic nuclei during stage 2 NREM sleep in a frequency range of ~11 to 16 Hz with a duration of 0.5 seconds or greater. After generation as an interaction of the TRN neurons and thalamocortical cells, spindles are sustained and relayed to the cortex by thalamo-thalamic and thalamo-cortical feedback loops regulated by both GABAergic and NMDA-receptor mediated glutamatergic neurotransmission. Sleep spindles have been reported for all tested mammalian species. Considering animals in which sleep-spindles were studied extensively, they appear to have a conserved main frequency of roughly 9–16 Hz. Only in humans, rats and dogs is a difference in the intrinsic frequency of frontal and posterior spindles confirmed, however.

Slow-wave sleep (SWS), often referred to as deep sleep, is the third stage of non-rapid eye movement sleep (NREM), where electroencephalography activity is characterised by slow delta waves.
Parasomnias are a category of sleep disorders that involve abnormal movements, behaviors, emotions, perceptions, and dreams that occur while falling asleep, sleeping, between sleep stages, or during arousal from sleep. Parasomnias are dissociated sleep states which are partial arousals during the transitions between wakefulness, NREM sleep, and REM sleep, and their combinations.
Rhythmic movement disorder (RMD) is a neurological disorder characterized by repetitive movements of large muscle groups immediately before and during sleep often involving the head and neck. It was independently described first in 1905 by Zappert as jactatio capitis nocturna and by Cruchet as rhythmie du sommeil. The majority of RMD episodes occur during NREM sleep, although REM movements have been reported. RMD is often associated with other psychiatric conditions or mental disabilities. The disorder often leads to bodily injury from unwanted movements. Because of these incessant muscle contractions, patients' sleep patterns are often disrupted. It differs from restless legs syndrome in that RMD involves involuntary muscle contractions before and during sleep while restless legs syndrome is the urge to move before sleep. RMD occurs in both males and females, often during early childhood with symptoms diminishing with age. Many affected individuals also have other sleep related disorders, like sleep apnea. The disorder can be differentially diagnosed into small subcategories, including sleep related bruxism, thumb sucking, hypnagogic foot tremor, and rhythmic sucking, to name a few. In order to be considered pathological, the ICSD-II requires that in the sleep-related rhythmic movements should “markedly interfere with normal sleep, cause significant impairment in daytime function, or result in self-inflicted bodily injury that requires medical treatment ”.
When we sleep, our breathing changes due to normal biological processes that affect both our respiratory and muscular systems.

Catathrenia or nocturnal groaning is a sleep-related breathing disorder, consisting of end-inspiratory apnea and expiratory groaning during sleep. It describes a rare condition characterized by monotonous, irregular groans while sleeping. Catathrenia begins with a deep inspiration. The person with catathrenia holds his or her breath against a closed glottis, similar to the Valsalva maneuver. Expiration can be slow and accompanied by sound caused by vibration of the vocal cords or a simple rapid exhalation. Despite a slower breathing rate, no oxygen desaturation usually occurs. The moaning sound is usually not noticed by the person producing the sound, but it can be extremely disturbing to sleep partners. It appears more often during expiration REM sleep than in NREM sleep.
Recurrent thalamo-cortical resonance or Thalamocortical oscillation is an observed phenomenon of oscillatory neural activity between the thalamus and various cortical regions of the brain. It is proposed by Rodolfo Llinas and others as a theory for the integration of sensory information into the whole of perception in the brain. Thalamocortical oscillation is proposed to be a mechanism of synchronization between different cortical regions of the brain, a process known as temporal binding. This is possible through the existence of thalamocortical networks, groupings of thalamic and cortical cells that exhibit oscillatory properties.
In neuroscience, the N100 or N1 is a large, negative-going evoked potential measured by electroencephalography ; it peaks in adults between 80 and 120 milliseconds after the onset of a stimulus, and is distributed mostly over the fronto-central region of the scalp. It is elicited by any unpredictable stimulus in the absence of task demands. It is often referred to with the following P200 evoked potential as the "N100-P200" or "N1-P2" complex. While most research focuses on auditory stimuli, the N100 also occurs for visual, olfactory, heat, pain, balance, respiration blocking, and somatosensory stimuli.

The relationship between sleep and memory has been studied since at least the early 19th century. Memory, the cognitive process of storing and retrieving past experiences, learning and recognition, is a product of brain plasticity, the structural changes within synapses that create associations between stimuli. Stimuli are encoded within milliseconds; however, the long-term maintenance of memories can take additional minutes, days, or even years to fully consolidate and become a stable memory that is accessible. Therefore, the formation of a specific memory occurs rapidly, but the evolution of a memory is often an ongoing process.

A hypnogram is a form of polysomnography; it is a graph that represents the stages of sleep as a function of time. It was developed as an easy way to present the recordings of the brain wave activity from an electroencephalogram (EEG) during a period of sleep. It allows the different stages of sleep: rapid eye movement sleep (REM) and non-rapid eye movement sleep (NREM) to be identified during the sleep cycle. NREM sleep can be further classified into NREM stage 1, 2 and 3. The previously considered 4th stage of NREM sleep has been included within stage 3; this stage is also called slow wave sleep (SWS) and is the deepest stage of sleep.

The neuroscience of sleep is the study of the neuroscientific and physiological basis of the nature of sleep and its functions. Traditionally, sleep has been studied as part of psychology and medicine. The study of sleep from a neuroscience perspective grew to prominence with advances in technology and the proliferation of neuroscience research from the second half of the twentieth century.