Related Research Articles

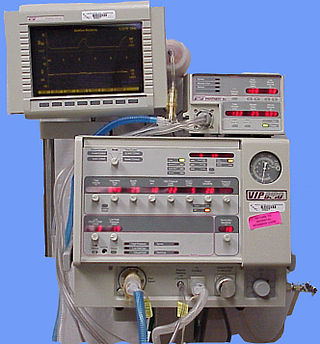
Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV), is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Tidal volume is the volume of air moved into or out of the lungs during a normal breath. In a healthy, young human adult, tidal volume is approximately 500 ml per inspiration or 7 ml/kg of body mass.

Barotrauma is physical damage to body tissues caused by a difference in pressure between a gas space inside, or contact with, the body and the surrounding gas or liquid. The initial damage is usually due to over-stretching the tissues in tension or shear, either directly by an expansion of the gas in the closed space or by pressure difference hydrostatically transmitted through the tissue. Tissue rupture may be complicated by the introduction of gas into the local tissue or circulation through the initial trauma site, which can cause blockage of circulation at distant sites or interfere with the normal function of an organ by its presence.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.
Salt water aspiration syndrome is a rare diving disorder suffered by scuba divers who inhale a mist of seawater, usually from a faulty demand valve, causing irritation of the lungs. It is not the same thing as aspiration of salt water as a bulk liquid, i.e. drowning. It can usually be treated by rest for several hours. If severe, medical assessment is required. First described by Carl Edmonds.

A bag valve mask (BVM), sometimes known by the proprietary name Ambu bag or generically as a manual resuscitator or "self-inflating bag", is a hand-held device commonly used to provide positive pressure ventilation to patients who are not breathing or not breathing adequately. The device is a required part of resuscitation kits for trained professionals in out-of-hospital settings (such as ambulance crews) and is also frequently used in hospitals as part of standard equipment found on a crash cart, in emergency rooms or other critical care settings. Underscoring the frequency and prominence of BVM use in the United States, the American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care recommend that "all healthcare providers should be familiar with the use of the bag-mask device." Manual resuscitators are also used within the hospital for temporary ventilation of patients dependent on mechanical ventilators when the mechanical ventilator needs to be examined for possible malfunction or when ventilator-dependent patients are transported within the hospital. Two principal types of manual resuscitators exist; one version is self-filling with air, although additional oxygen (O2) can be added but is not necessary for the device to function. The other principal type of manual resuscitator (flow-inflation) is heavily used in non-emergency applications in the operating room to ventilate patients during anesthesia induction and recovery.
Diving disorders, or diving related medical conditions, are conditions associated with underwater diving, and include both conditions unique to underwater diving, and those that also occur during other activities. This second group further divides into conditions caused by exposure to ambient pressures significantly different from surface atmospheric pressure, and a range of conditions caused by general environment and equipment associated with diving activities.
Permissive hypercapnia is hypercapnia in respiratory insufficient patients in which oxygenation has become so difficult that the optimal mode of mechanical ventilation is not capable of exchanging enough carbon dioxide. Carbon dioxide is a gaseous product of the body's metabolism and is normally expelled through the lungs.
Positive end-expiratory pressure (PEEP) is the pressure in the lungs above atmospheric pressure that exists at the end of expiration. The two types of PEEP are extrinsic PEEP and intrinsic PEEP. Pressure that is applied or increased during an inspiration is termed pressure support.PEEP is a therapeutic parameter set in the ventilator, or a complication of mechanical ventilation with air trapping (auto-PEEP).

Pneumomediastinum is pneumatosis in the mediastinum, the central part of the chest cavity. First described in 1819 by René Laennec, the condition can result from physical trauma or other situations that lead to air escaping from the lungs, airways, or bowel into the chest cavity. In underwater divers it is usually the result of pulmonary barotrauma.
High-frequency ventilation is a type of mechanical ventilation which utilizes a respiratory rate greater than four times the normal value. and very small tidal volumes. High frequency ventilation is thought to reduce ventilator-associated lung injury (VALI), especially in the context of ARDS and acute lung injury. This is commonly referred to as lung protective ventilation. There are different types of high-frequency ventilation. Each type has its own unique advantages and disadvantages. The types of HFV are characterized by the delivery system and the type of exhalation phase.
Ventilator-associated lung injury (VALI) is an acute lung injury that develops during mechanical ventilation and is termed ventilator-induced lung injury (VILI) if it can be proven that the mechanical ventilation caused the acute lung injury. In contrast, ventilator-associated lung injury (VALI) exists if the cause cannot be proven. VALI is the appropriate term in most situations because it is virtually impossible to prove what actually caused the lung injury in the hospital.
Neurally adjusted ventilatory assist (NAVA) is a mode of mechanical ventilation. NAVA delivers assistance in proportion to and in synchrony with the patient's respiratory efforts, as reflected by an electrical signal. This signal represents the electrical activity of the diaphragm, the body's principal breathing muscle.

Airway pressure release ventilation (APRV) is a pressure control mode of mechanical ventilation that utilizes an inverse ratio ventilation strategy. APRV is an applied continuous positive airway pressure (CPAP) that at a set timed interval releases the applied pressure. Depending on the ventilator manufacturer, it may be referred to as BiVent. This is just as appropriate to use, since the only difference is that the term APRV is copyrighted.

A liquid ventilator is similar to a medical ventilator except that it should be able to ensure reliable total liquid ventilation with a breatheable liquid ·. Liquid ventilators are prototypes that may have been used for animal experimentations but experts recommend continued development of a liquid ventilator toward clinical applications.
Continuous mandatory ventilation (CMV) is a mode of mechanical ventilation in which breaths are delivered based on set variables. Still used in the operating room, in previous nomenclature, CMV referred to "controlled mechanical ventilation", a mode of ventilation characterized by a ventilator that makes no effort to sense patient breathing effort. In continuous mandatory ventilation, the ventilator can be triggered either by the patient or mechanically by the ventilator. The ventilator is set to deliver a breath according to parameters selected by the operator. "Controlled mechanical ventilation" is an outdated expansion for "CMV"; "continuous mandatory ventilation" is now accepted standard nomenclature for mechanical ventilation. CMV today can assist or control itself dynamically, depending on the transient presence or absence of spontaneous breathing effort. Thus, today's CMV would have been called ACV in older nomenclature, and the original form of CMV is a thing of the past. But despite continual technological improvement over the past half century, CMV may still be uncomfortable for the patient.

Mechanical power is a medical term which is a measure of the amount of energy imparted to a patient by a mechanical ventilator.
Rheotrauma is a medical term for the harm caused to a patient's lungs by high gas flows as delivered by mechanical ventilation. Although mechanical ventilation may prevent death of a patient from the hypoxia or hypercarbia which may be caused by respiratory failure, it can also be damaging to the lungs, leading to ventilator-associated lung injury. Rheotrauma is one of the ways in which mechanical ventilation may do this, alongside volutrauma, barotrauma, atelectotrauma and biotrauma. Attempts have been made to combine all of the mechanical forces caused by the ventilator on the patient's lungs in an all encompassing term: mechanical power.

Atelectotrauma, atelectrauma, cyclic atelectasis or repeated alveolar collapse and expansion (RACE) are medical terms for the damage caused to the lung by mechanical ventilation under certain conditions. When parts of the lung collapse at the end of expiration, due to a combination of a diseased lung state and a low functional residual capacity, then reopen again on inspiration, this repeated collapsing and reopening causes shear stress which has a damaging effect on the alveolus. Clinicians attempt to reduce atelectotrauma by ensuring adequate positive end-expiratory pressure (PEEP) to maintain the alveoli open in expiration. This is known as open lung ventilation. High frequency oscillatory ventilation (HFOV) with its use of 'super CPAP' is especially effective in preventing atelectotrauma since it maintains a very high mean airway pressure (MAP), equivalent to a very high PEEP. Atelectotrauma is one of several means by which mechanical ventilation may damage the lungs leading to ventilator-associated lung injury. The other means are volutrauma, barotrauma, rheotrauma and biotrauma. Attempts have been made to combine these factors in an all encompassing term: mechanical power.
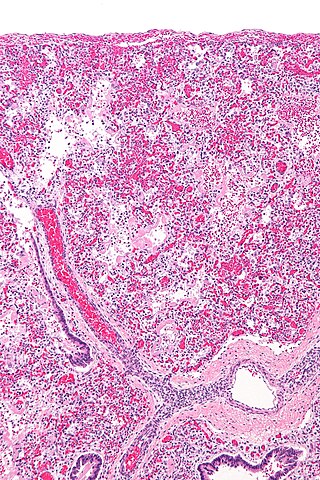
The pathophysiology of acute respiratory distress syndrome involves fluid accumulation in the lungs not explained by heart failure. It is typically provoked by an acute injury to the lungs that results in flooding of the lungs' microscopic air sacs responsible for the exchange of gases such as oxygen and carbon dioxide with capillaries in the lungs. Additional common findings in ARDS include partial collapse of the lungs (atelectasis) and low levels of oxygen in the blood (hypoxemia). The clinical syndrome is associated with pathological findings including pneumonia, eosinophilic pneumonia, cryptogenic organizing pneumonia, acute fibrinous organizing pneumonia, and diffuse alveolar damage (DAD). Of these, the pathology most commonly associated with ARDS is DAD, which is characterized by a diffuse inflammation of lung tissue. The triggering insult to the tissue usually results in an initial release of chemical signals and other inflammatory mediators secreted by local epithelial and endothelial cells.
References
- ↑ Halbertsma FJ, Vaneker M, Scheffer GJ, van der Hoeven JG (2005). "Cytokines and biotrauma in ventilator-induced lung injury: a critical review of the literature". Neth J Med. 63 (10): 382–92. PMID 16301759.
- ↑ Tremblay LN, Slutsky AS (1998). "Ventilator-induced injury: from barotrauma to biotrauma". Proc Assoc Am Physicians. 110 (6): 482–8. PMID 9824530.