Related Research Articles

A ventilator is a type of breathing apparatus, a class of medical technology that provides mechanical ventilation by moving breathable air into and out of the lungs, to deliver breaths to a patient who is physically unable to breathe, or breathing insufficiently. Ventilators may be computerized microprocessor-controlled machines, but patients can also be ventilated with a simple, hand-operated bag valve mask. Ventilators are chiefly used in intensive-care medicine, home care, and emergency medicine and in anesthesiology.

Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV) is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Respiratory arrest is a medical condition caused by apnea or respiratory dysfunction severe enough that it will not sustain the body. Prolonged apnea refers to a patient who has stopped breathing for a long period of time. If the heart muscle contraction is intact, the condition is known as respiratory arrest. An abrupt stop of pulmonary gas exchange lasting for more than five minutes may permanently damage vital organs, especially the brain. Lack of oxygen to the brain causes loss of consciousness. Brain injury is likely if respiratory arrest goes untreated for more than three minutes, and death is almost certain if more than five minutes.

A bag valve mask (BVM), sometimes known by the proprietary name Ambu bag or generically as a manual resuscitator or "self-inflating bag", is a hand-held device commonly used to provide positive pressure ventilation to patients who are not breathing or not breathing adequately. The device is a required part of resuscitation kits for trained professionals in out-of-hospital settings (such as ambulance crews) and is also frequently used in hospitals as part of standard equipment found on a crash cart, in emergency rooms or other critical care settings. Underscoring the frequency and prominence of BVM use in the United States, the American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care recommend that "all healthcare providers should be familiar with the use of the bag-mask device." Manual resuscitators are also used within the hospital for temporary ventilation of patients dependent on mechanical ventilators when the mechanical ventilator needs to be examined for possible malfunction or when ventilator-dependent patients are transported within the hospital. Two principal types of manual resuscitators exist; one version is self-filling with air, although additional oxygen (O2) can be added but is not necessary for the device to function. The other principal type of manual resuscitator (flow-inflation) is heavily used in non-emergency applications in the operating room to ventilate patients during anesthesia induction and recovery.
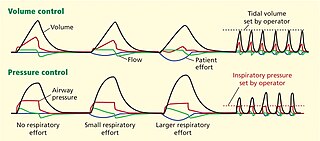
Dual-control modes of ventilation are auto-regulated pressure-controlled modes of mechanical ventilation with a user-selected tidal volume target. The ventilator adjusts the pressure limit of the next breath as necessary according to the previous breath's measured exhaled tidal volume. Peak airway pressure varies from breath to breath according to changes in the patient's airway resistance and lung compliance.
Positive end-expiratory pressure (PEEP) is the pressure in the lungs above atmospheric pressure that exists at the end of expiration. The two types of PEEP are extrinsic PEEP and intrinsic PEEP. Pressure that is applied or increased during an inspiration is termed pressure support.PEEP is a therapeutic parameter set in the ventilator, or a complication of mechanical ventilation with air trapping (auto-PEEP).
High-frequency ventilation is a type of mechanical ventilation which utilizes a respiratory rate greater than four times the normal value. and very small tidal volumes. High frequency ventilation is thought to reduce ventilator-associated lung injury (VALI), especially in the context of ARDS and acute lung injury. This is commonly referred to as lung protective ventilation. There are different types of high-frequency ventilation. Each type has its own unique advantages and disadvantages. The types of HFV are characterized by the delivery system and the type of exhalation phase.
Ventilator-associated lung injury (VALI) is an acute lung injury that develops during mechanical ventilation and is termed ventilator-induced lung injury (VILI) if it can be proven that the mechanical ventilation caused the acute lung injury. In contrast, ventilator-associated lung injury (VALI) exists if the cause cannot be proven. VALI is the appropriate term in most situations because it is virtually impossible to prove what actually caused the lung injury in the hospital.
Neurally adjusted ventilatory assist (NAVA) is a mode of mechanical ventilation. NAVA delivers assistance in proportion to and in synchrony with the patient's respiratory efforts, as reflected by an electrical signal. This signal represents the electrical activity of the diaphragm, the body's principal breathing muscle.
Pressure support ventilation (PSV), also known as pressure support, is a spontaneous mode of ventilation. The patient initiates every breath and the ventilator delivers support with the preset pressure value. With support from the ventilator, the patient also regulates their own respiratory rate and tidal volume.
Pressure control (PC) is a mode of mechanical ventilation alone and a variable within other modes of mechanical ventilation. Pressure control is used to regulate pressures applied during mechanical ventilation. Air delivered into the patients lungs (breaths) are currently regulated by Volume Control or Pressure Control. In pressure controlled breaths a tidal volume achieved is based on how much volume can be delivered before the pressure control limit is reached.

Airway pressure release ventilation (APRV) is a pressure control mode of mechanical ventilation that utilizes an inverse ratio ventilation strategy. APRV is an applied continuous positive airway pressure (CPAP) that at a set timed interval releases the applied pressure. Depending on the ventilator manufacturer, it may be referred to as BiVent. This is just as appropriate to use, since the only difference is that the term APRV is copyrighted.

A liquid ventilator is similar to a medical ventilator except that it should be able to ensure reliable total liquid ventilation with a breatheable liquid ·. Liquid ventilators are prototypes that may have been used for animal experimentations but experts recommend continued development of a liquid ventilator toward clinical applications.
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy.
Many terms are used in mechanical ventilation, some are specific to brand, model, trademark and mode of mechanical ventilation. There is a standardized nomenclature of mechanical ventilation that is specific about nomenclature related to modes, but not settings and variables.
Mandatory minute ventilation (MMV) is a mode of mechanical ventilation which requires the operator to determine what the appropriate minute ventilation for the patient should be and the ventilator then monitors the patient's ability to generate this volume. If the calculation suggests the volume target will not be met, supplemental breaths are delivered at the targeted volume to achieve the desired minute ventilation.
Intermittent Mandatory Ventilation (IMV) refers to any mode of mechanical ventilation where a regular series of breaths are scheduled but the ventilator senses patient effort and reschedules mandatory breaths based on the calculated need of the patient. Similar to continuous mandatory ventilation in parameters set for the patients pressures and volumes but distinct in its ability to support a patient by either supporting their own effort or providing support when patient effort is not sensed. IMV is frequently paired with additional strategies to improve weaning from ventilator support or to improve cardiovascular stability in patients who may need full life support.

The SensorMedics High-Frequency Oscillatory Ventilator is a patented high-frequency mechanical ventilator designed and manufactured by SensorMedics Corp. of Yorba Linda, California. After a series of acquisitions, Vyaire Medical, Inc. marketed the product as 3100A/B HFOV Ventilators. Model 3100 received premarket approval from the United States Food and Drug Administration (FDA) in 1991 for treatment of all forms of respiratory failure in neonatal patients. In 1995, it received pre-market approved for Pediatric Application with no upper weight limit for treating selected patients failing on conventional ventilation.
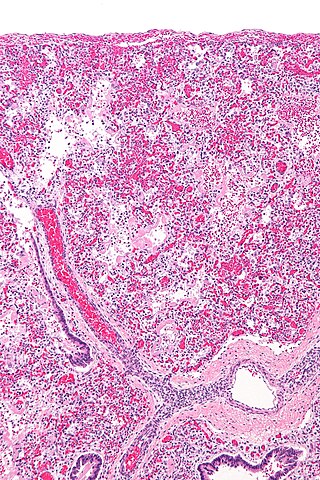
The pathophysiology of acute respiratory distress syndrome involves fluid accumulation in the lungs not explained by heart failure. It is typically provoked by an acute injury to the lungs that results in flooding of the lungs' microscopic air sacs responsible for the exchange of gases such as oxygen and carbon dioxide with capillaries in the lungs. Additional common findings in ARDS include partial collapse of the lungs (atelectasis) and low levels of oxygen in the blood (hypoxemia). The clinical syndrome is associated with pathological findings including pneumonia, eosinophilic pneumonia, cryptogenic organizing pneumonia, acute fibrinous organizing pneumonia, and diffuse alveolar damage (DAD). Of these, the pathology most commonly associated with ARDS is DAD, which is characterized by a diffuse inflammation of lung tissue. The triggering insult to the tissue usually results in an initial release of chemical signals and other inflammatory mediators secreted by local epithelial and endothelial cells.
References
- ↑ Sassoon CS, Zhu E, Caiozzo VJ (2004). "Assist-control mechanical ventilation attenuates ventilator-induced diaphragmatic dysfunction". Am J Respir Crit Care Med. 170 (6): 626–32. doi:10.1164/rccm.200401-042OC. PMID 15201132.
- ↑ Macintyre N (2011). "Counterpoint: Is Pressure Assist-Control Preferred Over Volume Assist-Control Mode for Lung Protective Ventilation in Patients With ARDS? No". Chest. 140 (2): 290–2. doi: 10.1378/chest.11-1052 . PMID 21813526.
- ↑ MAQUET, "Modes of ventilation in SERVO-i, Invasive and Non-invasive, 2008 MAQUET Critical Care AB, Order No 66 14 692
- ↑ MAQUET, "Modes of ventilation in SERVO-s, Invasive and Non-invasive", 2009 MAQUET Critical Care AB, Order No 66 61 131
- 1 2 Chatburn RL. Classification of ventilator modes: update and proposal for implementation. Respir Care 2007; 52:301–323. PMID 17328828