Mechanical ventilation or assisted ventilation is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.

Spirometry is the most common of the pulmonary function tests (PFTs). It measures lung function, specifically the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is helpful in assessing breathing patterns that identify conditions such as asthma, pulmonary fibrosis, cystic fibrosis, and COPD. It is also helpful as part of a system of health surveillance, in which breathing patterns are measured over time.
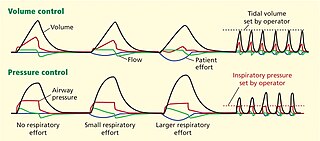
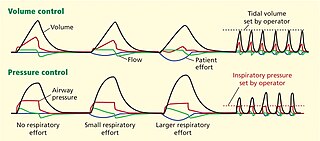
Dual-control modes of ventilation are auto-regulated pressure-controlled modes of mechanical ventilation with a user-selected tidal volume target. The ventilator adjusts the pressure limit of the next breath as necessary according to the previous breath's measured exhaled tidal volume. Peak airway pressure varies from breath to breath according to changes in the patient's airway resistance and lung compliance.
Positive end-expiratory pressure (PEEP) is the pressure in the lungs above atmospheric pressure that exists at the end of expiration. The two types of PEEP are extrinsic PEEP and intrinsic PEEP. Pressure that is applied or increased during an inspiration is termed pressure support.PEEP is a therapeutic parameter set in the ventilator, or a complication of mechanical ventilation with air trapping (auto-PEEP).
High-frequency ventilation is a type of mechanical ventilation which utilizes a respiratory rate greater than four times the normal value. and very small tidal volumes. High frequency ventilation is thought to reduce ventilator-associated lung injury (VALI), especially in the context of ARDS and acute lung injury. This is commonly referred to as lung protective ventilation. There are different types of high-frequency ventilation. Each type has its own unique advantages and disadvantages. The types of HFV are characterized by the delivery system and the type of exhalation phase.
In respiratory physiology, airway resistance is the resistance of the respiratory tract to airflow during inhalation and exhalation. Airway resistance can be measured using plethysmography.
Lung compliance, or pulmonary compliance, is a measure of the lung's ability to stretch and expand. In clinical practice it is separated into two different measurements, static compliance and dynamic compliance. Static lung compliance is the change in volume for any given applied pressure. Dynamic lung compliance is the compliance of the lung at any given time during actual movement of air.

Pulmonary function testing (PFT) is a complete evaluation of the respiratory system including patient history, physical examinations, and tests of pulmonary function. The primary purpose of pulmonary function testing is to identify the severity of pulmonary impairment. Pulmonary function testing has diagnostic and therapeutic roles and helps clinicians answer some general questions about patients with lung disease. PFTs are normally performed by a pulmonary function technician, respiratory therapist, respiratory physiologist, physiotherapist, pulmonologist, or general practitioner.

Airway pressure release ventilation (APRV) is a pressure control mode of mechanical ventilation that utilizes an inverse ratio ventilation strategy. APRV is an applied continuous positive airway pressure (CPAP) that at a set timed interval releases the applied pressure. Depending on the ventilator manufacturer, it may be referred to as BiVent. This is just as appropriate to use, since the only difference is that the term APRV is copyrighted.

A liquid ventilator is similar to a medical ventilator except that it should be able to ensure reliable total liquid ventilation with a breatheable liquid ·. Liquid ventilators are prototypes that may have been used for animal experimentations but experts recommend continued development of a liquid ventilator toward clinical applications.

Heated humidified high-flow therapy, often simply called high flow therapy, is a type of respiratory support that delivers a flow of medical gas to a patient of up to 60 liters per minute and 100% oxygen through a large bore or high flow nasal cannula. Primarily studied in neonates, it has also been found effective in some adults to treat hypoxemia and work of breathing issues. The key components of it are a gas blender, heated humidifier, heated circuit, and cannula.
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy.
ΔP is a mathematical term symbolizing a change (Δ) in pressure (P).
Many terms are used in mechanical ventilation, some are specific to brand, model, trademark and mode of mechanical ventilation. There is a standardized nomenclature of mechanical ventilation that is specific about nomenclature related to modes, but not settings and variables.
Inverse ratio ventilation (IRV) is not necessarily a mode of mechanical ventilation though it may be referred to as such. IRV is a strategy of ventilating the lungs in such a way that the amount of time the lungs are in inhalation is greater than the amount of time they are in exhalation, allowing for a constant inflation of the lungs, ensuring they remain "recruited". The primary goal for IRV is improved oxygenation by forcing inspiratory time to be greater than expiratory time increasing the mean airway pressure and potentially improving oxygenation. Normal I:E ratio is 5:6, so forcing the I:E to be 2:1, 3:1, 4:1, is the source of the term for the strategy.
Peak inspiratory pressure (PIP) is the highest level of pressure applied to the lungs during inhalation. In mechanical ventilation the number reflects a positive pressure in centimeters of water pressure (cm H2O). In normal breathing, it may sometimes be referred to as the maximal inspiratory pressure (MIPO), which is a negative value.
The oxygenation index is a calculation used in intensive care medicine to measure the fraction of inspired oxygen (FiO2) and its usage within the body.

Atelectotrauma, atelectrauma, cyclic atelectasis or repeated alveolar collapse and expansion (RACE) are medical terms for the damage caused to the lung by mechanical ventilation under certain conditions. When parts of the lung collapse at the end of expiration, due to a combination of a diseased lung state and a low functional residual capacity, then reopen again on inspiration, this repeated collapsing and reopening causes shear stress which has a damaging effect on the alveolus. Clinicians attempt to reduce atelectotrauma by ensuring adequate positive end-expiratory pressure (PEEP) to maintain the alveoli open in expiration. This is known as open lung ventilation. High frequency oscillatory ventilation (HFOV) with its use of 'super CPAP' is especially effective in preventing atelectotrauma since it maintains a very high mean airway pressure (MAP), equivalent to a very high PEEP. Atelectotrauma is one of several means by which mechanical ventilation may damage the lungs leading to ventilator-associated lung injury. The other means are volutrauma, barotrauma, rheotrauma and biotrauma. Attempts have been made to combine these factors in an all encompassing term: mechanical power.
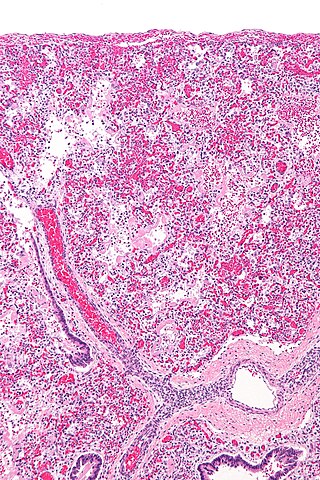
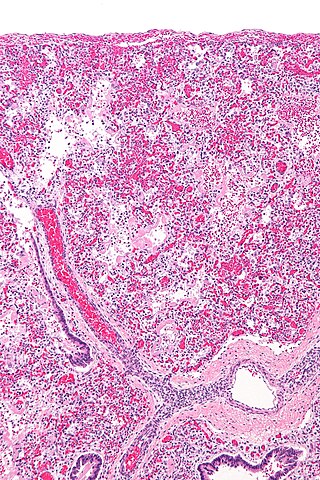
The pathophysiology of acute respiratory distress syndrome involves fluid accumulation in the lungs not explained by heart failure. It is typically provoked by an acute injury to the lungs that results in flooding of the lungs' microscopic air sacs responsible for the exchange of gases such as oxygen and carbon dioxide with capillaries in the lungs. Additional common findings in ARDS include partial collapse of the lungs (atelectasis) and low levels of oxygen in the blood (hypoxemia). The clinical syndrome is associated with pathological findings including pneumonia, eosinophilic pneumonia, cryptogenic organizing pneumonia, acute fibrinous organizing pneumonia, and diffuse alveolar damage (DAD). Of these, the pathology most commonly associated with ARDS is DAD, which is characterized by a diffuse inflammation of lung tissue. The triggering insult to the tissue usually results in an initial release of chemical signals and other inflammatory mediators secreted by local epithelial and endothelial cells.