Related Research Articles
Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV), is the medical term for artificial ventilation where mechanical means are used to assist or replace spontaneous breathing. This may involve a machine called a ventilator, or the breathing may be assisted manually by a suitably qualified professional, such as an anesthesiologist, registered nurse (RN), paramedic or other first responder, or in some parts of the United States, by a respiratory therapist (RT), by compressing a bag valve mask device.

Positive airway pressure (PAP) is a mode of respiratory ventilation used in the treatment of sleep apnea. PAP ventilation is also commonly used for those who are critically ill in hospital with respiratory failure, in newborn infants (neonates), and for the prevention and treatment of atelectasis in patients with difficulty taking deep breaths. In these patients, PAP ventilation can prevent the need for tracheal intubation, or allow earlier extubation. Sometimes patients with neuromuscular diseases use this variety of ventilation as well. CPAP is an acronym for "continuous positive airway pressure", which was developed by Dr. George Gregory and colleagues in the neonatal intensive care unit at the University of California, San Francisco. A variation of the PAP system was developed by Professor Colin Sullivan at Royal Prince Alfred Hospital in Sydney, Australia, in 1981.

Respiratory arrest is caused by apnea or respiratory dysfunction severe enough it will not sustain the body. Prolonged apnea refers to a patient who has stopped breathing for a long period of time. If the heart muscle contraction is intact, the condition is known as respiratory arrest. An abrupt stop of pulmonary gas exchange lasting for more than five minutes may damage vital organs especially the brain, possibly permanently. Lack of oxygen to the brain causes loss of consciousness. Brain injury is likely if respiratory arrest goes untreated for more than three minutes, and death is almost certain if more than five minutes.

Non-invasive ventilation (NIV) is the use of breathing support administered through a face mask, nasal mask, or a helmet. Air, usually with added oxygen, is given through the mask under positive pressure; generally the amount of pressure is alternated depending on whether someone is breathing in or out. It is termed "non-invasive" because it is delivered with a mask that is tightly fitted to the face or around the head, but without a need for tracheal intubation. While there are similarities with regards to the interface, NIV is not the same as continuous positive airway pressure (CPAP), which applies a single level of positive airway pressure throughout the whole respiratory cycle; CPAP does not deliver ventilation but is occasionally used in conditions also treated with NIV.

A bag valve mask (BVM), sometimes known by the proprietary name Ambu bag or generically as a manual resuscitator or "self-inflating bag", is a hand-held device commonly used to provide positive pressure ventilation to patients who are not breathing or not breathing adequately. The device is a required part of resuscitation kits for trained professionals in out-of-hospital settings (such as ambulance crews) and is also frequently used in hospitals as part of standard equipment found on a crash cart, in emergency rooms or other critical care settings. Underscoring the frequency and prominence of BVM use in the United States, the American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care recommend that "all healthcare providers should be familiar with the use of the bag-mask device." Manual resuscitators are also used within the hospital for temporary ventilation of patients dependent on mechanical ventilators when the mechanical ventilator needs to be examined for possible malfunction or when ventilator-dependent patients are transported within the hospital. Two principal types of manual resuscitators exist; one version is self-filling with air, although additional oxygen (O2) can be added but is not necessary for the device to function. The other principal type of manual resuscitator (flow-inflation) is heavily used in non-emergency applications in the operating room to ventilate patients during anesthesia induction and recovery.
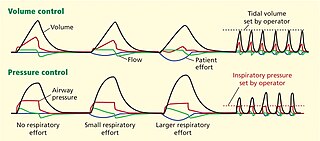
Dual-control modes of ventilation are auto-regulated pressure-controlled modes of mechanical ventilation with a user-selected tidal volume target. The ventilator adjusts the pressure limit of the next breath as necessary according to the previous breath's measured exhaled tidal volume. Peak airway pressure varies from breath to breath according to changes in the patient's airway resistance and lung compliance.
Positive end-expiratory pressure (PEEP) is the pressure in the lungs above atmospheric pressure that exists at the end of expiration. The two types of PEEP are extrinsic PEEP and intrinsic PEEP. Pressure that is applied or increased during an inspiration is termed pressure support.
High-frequency ventilation is a type of mechanical ventilation which utilizes a respiratory rate greater than four times the normal value. and very small tidal volumes. High frequency ventilation is thought to reduce ventilator-associated lung injury (VALI), especially in the context of ARDS and acute lung injury. This is commonly referred to as lung protective ventilation. There are different types of high-frequency ventilation. Each type has its own unique advantages and disadvantages. The types of HFV are characterized by the delivery system and the type of exhalation phase.
A goal for most patients on mechanical ventilation is to be weaned from the ventilator. The weaning process is highly dependent on the patient's pathology, but the final common pathway to ventilator independence always includes at least one trial of spontaneous breathing. Trials of spontaneous breathing have been shown to accurately predict the success of spontaneous breathing.
Pressure support ventilation (PSV), also known as pressure support, is a spontaneous mode of ventilation. The patient initiates every breath and the ventilator delivers support with the preset pressure value. With support from the ventilator, the patient also regulates his own respiratory rate and tidal volume.
Pressure control (PC) is a mode of mechanical ventilation alone and a variable within other modes of mechanical ventilation. Pressure control is used to regulate pressures applied during mechanical ventilation. Air delivered into the patients lungs (breaths) are currently regulated by Volume Control or Pressure Control. In pressure controlled breaths a tidal volume achieved is based on how much volume can be delivered before the pressure control limit is reached.

Airway pressure release ventilation (APRV) is a pressure control mode of mechanical ventilation that utilizes an inverse ratio ventilation strategy. APRV is an applied continuous positive airway pressure (CPAP) that at a set timed interval releases the applied pressure. Depending on the ventilator manufacturer, it may be referred to as BiVent. This is just as appropriate to use, since the only difference is that the term APRV is copyrighted.
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy.
The rapid shallow breathing index (RSBI) is a tool that is used in the weaning of mechanical ventilation on intensive care units. The RSBI is defined as the ratio of respiratory frequency to tidal volume (f/VT). People on a ventilator who cannot tolerate independent breathing tend to breathe rapidly and shallowly, and will therefore have a high RSBI.
Continuous mandatory ventilation (CMV) is a mode of mechanical ventilation in which breaths are delivered based on set variables. Still used in the operating room, in previous nomenclature CMV referred to "controlled mechanical ventilation", a mode of ventilation characterized by a ventilator that makes no effort to sense patient breathing effort. In continuous mandatory ventilation, the ventilator can be triggered either by the patient or mechanically by the ventilator. The ventilator is set to deliver a breath according to parameters selected by the operator. "Controlled mechanical ventilation" is an outdated expansion for "CMV"; "continuous mandatory ventilation" is now accepted standard nomenclature of mechanical ventilation. CMV today can assist or control dynamically, depending on transient presence or absence of spontaneous breathing effort. Thus, today's CMV would have been called ACV in older nomenclature, and the original form of CMV is a thing of the past. But despite continual technological improvement over the past half century, CMV sometimes may still be uncomfortable for the patient.
Many terms are used in mechanical ventilation, some are specific to brand, model, trademark and mode of mechanical ventilation. There is a standardized nomenclature of mechanical ventilation that is specific about nomenclature related to modes, but not settings and variables.
Intermittent Mandatory Ventilation (IMV) refers to any mode of mechanical ventilation where a regular series of breaths are scheduled but the ventilator senses patient effort and reschedules mandatory breaths based on the calculated need of the patient. Similar to continuous mandatory ventilation in parameters set for the patients pressures and volumes but distinct in its ability to support a patient by either supporting their own effort or providing support when patient effort is not sensed. IMV is frequently paired with additional strategies to improve weaning from ventilator support or to improve cardiovascular stability in patients who may need full life support.
Dynamic hyperinflation is a phenomenon that occurs when a new breath begins before the lung has reached the static equilibrium volume.
A negative pressure ventilator (NPV) is a type of mechanical ventilator that stimulates an ill person's breathing by periodically applying negative air pressure to their body to expand and contract the chest cavity.
Airway clearance therapy is treatment that uses a number of airway clearance techniques to clear the respiratory airways of mucus and other secretions. Several respiratory diseases cause the normal mucociliary clearance mechanism to become impaired resulting in a build-up of mucus which obstructs breathing, and also affects the cough reflex. Mucus build-up can also cause infection, and inflammation, and repeated infections can result in damage to the airways, and the lung tissue.
References
- ↑ Modrykamien A, Chatburn RL, Ashton RW (February 2011). "Airway pressure release ventilation: an alternative mode of mechanical ventilation in acute respiratory distress syndrome". Cleveland Clinic Journal of Medicine . 78 (2): 101–10. doi: 10.3949/ccjm.78a.10032 . PMID 21285342.