Related Research Articles

In histology, osteoid is the unmineralized, organic portion of the bone matrix that forms prior to the maturation of bone tissue. Osteoblasts begin the process of forming bone tissue by secreting the osteoid as several specific proteins. When it becomes mineralized, the osteoid and its adjacent bone cells have developed into new bone tissue.

Itch is a sensation that causes a strong desire or reflex to scratch. Itches have resisted many attempts to be classified as any one type of sensory experience. Itches have many similarities to pain, and while both are unpleasant sensory experiences, their behavioral response patterns are different. Pain creates a withdrawal reflex, whereas itches leads to a scratch reflex.
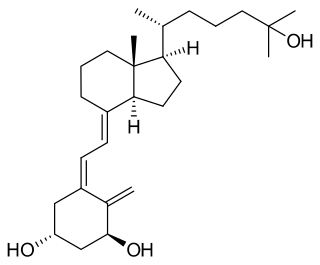
Osteomalacia is a disease characterized by the softening of the bones caused by impaired bone metabolism primarily due to inadequate levels of available phosphate, calcium, and vitamin D, or because of resorption of calcium. The impairment of bone metabolism causes inadequate bone mineralization.

A nociceptor is a sensory neuron that responds to damaging or potentially damaging stimuli by sending "possible threat" signals to the spinal cord and the brain. The brain creates the sensation of pain to direct attention to the body part, so the threat can be mitigated; this process is called nociception.

The human musculoskeletal system is an organ system that gives humans the ability to move using their muscular and skeletal systems. The musculoskeletal system provides form, support, stability, and movement to the body.
Renal osteodystrophy is currently defined as an alteration of bone morphology in patients with chronic kidney disease (CKD). It is one measure of the skeletal component of the systemic disorder of chronic kidney disease-mineral and bone disorder (CKD-MBD). The term "renal osteodystrophy" was coined in 1943, 60 years after an association was identified between bone disease and kidney failure.

Hypophosphatasia (; also called deficiency of alkaline phosphatase, phosphoethanolaminuria, or Rathbun's syndrome; sometimes abbreviated HPP) is a rare, and sometimes fatal, inherited metabolic bone disease. Clinical symptoms are heterogeneous, ranging from the rapidly fatal, perinatal variant, with profound skeletal hypomineralization, respiratory compromise or vitamin B6 dependent seizures to a milder, progressive osteomalacia later in life. Tissue non-specific alkaline phosphatase (TNSALP) deficiency in osteoblasts and chondrocytes impairs bone mineralization, leading to rickets or osteomalacia. The pathognomonic finding is subnormal serum activity of the TNSALP enzyme, which is caused by one of 388 genetic mutations identified to date, in the gene encoding TNSALP. Genetic inheritance is autosomal recessive for the perinatal and infantile forms but either autosomal recessive or autosomal dominant in the milder forms.

Allodynia is a condition in which pain is caused by a stimulus that does not normally elicit pain. For example, sunburn can cause temporary allodynia, so that usually painless stimuli, such as wearing clothing or running cold or warm water over it, can be very painful. It is different from hyperalgesia, an exaggerated response from a normally painful stimulus. The term comes from Ancient Greek άλλος (állos) 'other', and οδύνη (odúnē) 'pain'.

The neuroimmune system is a system of structures and processes involving the biochemical and electrophysiological interactions between the nervous system and immune system which protect neurons from pathogens. It serves to protect neurons against disease by maintaining selectively permeable barriers, mediating neuroinflammation and wound healing in damaged neurons, and mobilizing host defenses against pathogens.
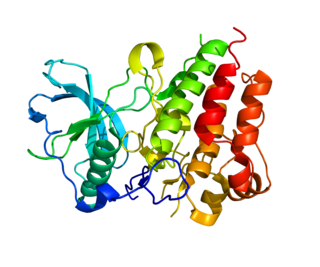
Receptor activator of nuclear factor kappa-Β ligand (RANKL), also known as tumor necrosis factor ligand superfamily member 11 (TNFSF11), TNF-related activation-induced cytokine (TRANCE), osteoprotegerin ligand (OPGL), and osteoclast differentiation factor (ODF), is a protein that in humans is encoded by the TNFSF11 gene.

Group C nerve fibers are one of three classes of nerve fiber in the central nervous system (CNS) and peripheral nervous system (PNS). The C group fibers are unmyelinated and have a small diameter and low conduction velocity, whereas Groups A and B are myelinated. Group C fibers include postganglionic fibers in the autonomic nervous system (ANS), and nerve fibers at the dorsal roots. These fibers carry sensory information.

Hydroxycarboxylic acid receptor 2 (HCA2), also known as GPR109A and niacin receptor 1 (NIACR1), is a protein which in humans is encoded (its formation is directed) by the HCAR2 gene and in rodents by the Hcar2 gene. The human HCAR2 gene is located on the long (i.e., "q") arm of chromosome 12 at position 24.31 (notated as 12q24.31). Like the two other hydroxycarboxylic acid receptors, HCA1 and HCA3, HCA2 is a G protein-coupled receptor (GPCR) located on the surface membrane of cells. HCA2 binds and thereby is activated by D-β-hydroxybutyric acid (hereafter termed β-hydroxybutyric acid), butyric acid, and niacin (also known as nicotinic acid). β-Hydroxybutyric and butyric acids are regarded as the endogenous agents that activate HCA2. Under normal conditions, niacin's blood levels are too low to do so: it is given as a drug in high doses in order to reach levels that activate HCA2.
Colony stimulating factor 1 receptor (CSF1R), also known as macrophage colony-stimulating factor receptor (M-CSFR), and CD115, is a cell-surface protein encoded by the human CSF1R gene. CSF1R is a receptor that can be activated by two ligands: colony stimulating factor 1 (CSF-1) and interleukin-34 (IL-34). CSF1R is highly expressed in myeloid cells, and CSF1R signaling is necessary for the survival, proliferation, and differentiation of many myeloid cell types in vivo and in vitro. CSF1R signaling is involved in many diseases and is targeted in therapies for cancer, neurodegeneration, and inflammatory bone diseases.
Oncogenic osteomalacia, also known as oncogenic hypophosphatemic osteomalacia, is an uncommon disorder resulting in increased renal phosphate excretion, hypophosphatemia and osteomalacia. It may be caused by a phosphaturic mesenchymal tumor.

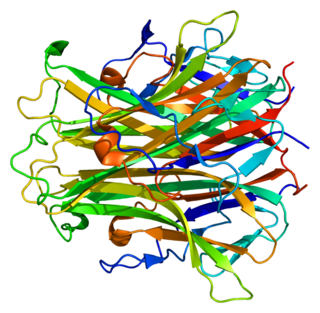
Elevated alkaline phosphatase occurs when levels of alkaline phosphatase (ALP) exceed the reference range. This group of enzymes has a low substrate specificity and catalyzes the hydrolysis of phosphate esters in a basic environment. The major function of alkaline phosphatase is transporting chemicals across cell membranes. Alkaline phosphatases are present in many human tissues, including bone, intestine, kidney, liver, placenta and white blood cells. Damage to these tissues causes the release of ALP into the bloodstream. Elevated levels can be detected through a blood test. Elevated alkaline phosphate is associated with certain medical conditions or syndromes. It serves as a significant indicator for certain medical conditions, diseases and syndromes.

Bone metastasis, or osseous metastatic disease, is a category of cancer metastases that result from primary tumor invasions into bones. Bone-originating primary tumors such as osteosarcoma, chondrosarcoma, and Ewing sarcoma are rare; the most common bone tumor is a metastasis. Bone metastases can be classified as osteolytic, osteoblastic, or both. Unlike hematologic malignancies which originate in the blood and form non-solid tumors, bone metastases generally arise from epithelial tumors and form a solid mass inside the bone. Bone metastases, especially in a state of advanced disease, can cause severe pain, characterized by a dull, constant ache with periodic spikes of incident pain.
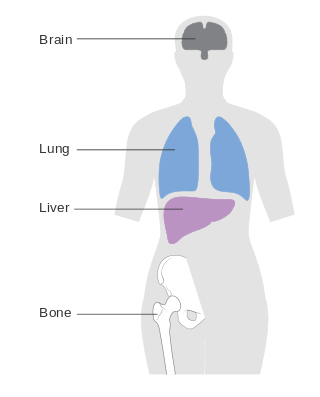
Metastatic breast cancer, also referred to as metastases, advanced breast cancer, secondary tumors, secondaries or stage IV breast cancer, is a stage of breast cancer where the breast cancer cells have spread to distant sites beyond the axillary lymph nodes. There is no cure for metastatic breast cancer; there is no stage after IV.
Group A nerve fibers are one of the three classes of nerve fiber as generally classified by Erlanger and Gasser. The other two classes are the group B nerve fibers, and the group C nerve fibers. Group A are heavily myelinated, group B are moderately myelinated, and group C are unmyelinated.
Cancer pain can be caused by pressure on, or chemical stimulation of, specialised pain-signalling nerve endings called nociceptors, or by damage or illness affecting nerve fibers themselves.

An osteolytic lesion is a softened section of a patient's bone formed as a symptom of specific diseases, including breast cancer and multiple myeloma. This softened area appears as a hole on X-ray scans due to decreased bone density, although many other diseases are associated with this symptom. Osteolytic lesions can cause pain, increased risk of bone fracture, and spinal cord compression. These lesions can be treated using biophosphonates or radiation, though new solutions are being tested in clinical trials.
References
- 1 2 3 4 Luger, N. Mach, D. Sevcik, M. Mantyh, P. (2005). Bone cancer pain: From mechanism to model to therapy. Journal of Pain and Symptom Management. 29(5): 32-46.
- ↑ Zwas, T. Elkanovitch, R. George, F. (1987). Interpretation and Classification of Bone Scintigraphic Findings in Stress Fractures. Journal of Nuclear Medicine. 28: 452-457.
- 1 2 3 Mantyh, P. Clohisy, D. Koltzenburg, M. Hunt, S. (2002). Molecular Mechanism of Cancer Pain. Nature Reviews Cancer. 2: 201-209.
- 1 2 McCredie J (2007). Nerves in bone: the silent partners. Skeletal Radiology. 36: 473–475.
- 1 2 3 Mach, D. Rogers, S. Sabino, M. Luger, N. Schwei, M. Pomonis, J. Keyser, C. Clohisy, D. Adams, D. O'leary, P. Mantyh, P. (2002). Origins of skeletal pain: Sensory and sympathetic innervation of the mouse femur. Neuroscience. 113(1):155-166.
- ↑ Falk S, Uldall M, Heegaard AM. (2012). The role of purinergic receptors in cancer-induced bone pain. J Osteoporos. 2012;2012:758181. doi: 10.1155/2012/758181
- 1 2 3 4 5 6 7 8 9 10 11 Mantyh PW (2014). "The neurobiology of skeletal pain". Eur J Neurosci (Review). 39 (3): 508–19. doi:10.1111/ejn.12462. PMC 4453827 . PMID 24494689.
- 1 2 Leffler DA, Green PH, Fasano A (Oct 2015). "Extraintestinal manifestations of coeliac disease". Nat Rev Gastroenterol Hepatol (Review). 12 (10): 561–71. doi:10.1038/nrgastro.2015.131. PMID 26260366. S2CID 15561525.
- ↑ Aziz I, Hadjivassiliou M, Sanders DS (Sep 2015). "The spectrum of noncoeliac gluten sensitivity". Nat Rev Gastroenterol Hepatol (Review). 12 (9): 516–26. doi:10.1038/nrgastro.2015.107. PMID 26122473. S2CID 2867448.
- 1 2 3 4 5 6 7 Junnila JL, Cartwright VW (2006). "Chronic musculoskeletal pain in children: part II. Rheumatic causes". Am Fam Physician. 74 (2): 293–300. PMID 16883927.
- ↑ Buskila D, Ablin J (2012). "Pediatric fibromyalgia". Reumatismo (Review). 64 (4): 230–7. doi: 10.4081/reumatismo.2012.230 . PMID 23024967. S2CID 6689576.
- ↑ Uziel Y, Hashkes PJ (2007). "Growing pains in children". Pediatric Rheumatology Online Journal. 5: 5. doi: 10.1186/1546-0096-5-5 . PMC 1869025 . PMID 17550631.
- 1 2 3 4 5 6 Junnila JL, Cartwright VW (2006). "Chronic musculoskeletal pain in children: part I. Initial evaluation". Am Fam Physician (Review). 74 (1): 115–22. PMID 16848385.
- 1 2 3 4 5 Ajdinovic B, Jaukovic L, Antoniou D (2013). "Five benign myoskeletal diseases in paediatrics and the role of nuclear medicine. Do they differ from those in adults?". Hell J Nucl Med. 16 (1): 2–8. PMID 23529387.
- ↑ Hazzazi MA, Alzeer I, Tamimi W, Al Atawi M, Al Alwan I (2013). "Clinical presentation and etiology of osteomalacia/rickets in adolescents". Saudi Journal of Kidney Diseases and Transplantation. 24 (5): 938–41. doi: 10.4103/1319-2442.118087 . PMID 24029258.
- ↑ "Septic Arthritis". The Lecturio Medical Concept Library. Retrieved 27 August 2021.
- ↑ von Moos, R. Strasser, F. Gillessen, S. Zaugg, K. (2008). Metastatic bone pain: treatment options with an emphasis on bisphosphonates. Supportive Care in Cancer. 16(10): 1105-1115.
- 1 2 Mercadante, S. (1997). Malignant bone pain: Pathophysiology and treatment. Pain. 69(1-2):1-18.
- ↑ Furuse, S. Kawamata, T. Yamamoto, J. Niiyama, Y. Omote, K. Watanabe, M. Namiki, A.(2009). Reduction of Bone Cancer Pain by Activation of Spinal Cannabinoid Receptor 1 and Its Expression in the Superficial Dorsal Horn of the Spinal Cord in a Murine Model of Bone Cancer Pain. Anesthesiology. 111: 173–86.