Osteopetrosis, literally "stone bone", also known as marble bone disease or Albers-Schönberg disease, is an extremely rare inherited disorder whereby the bones harden, becoming denser, in contrast to more prevalent conditions like osteoporosis, in which the bones become less dense and more brittle, or osteomalacia, in which the bones soften. Osteopetrosis can cause bones to dissolve and break.

Café au lait spots, or café au lait macules, are flat, hyperpigmented birthmarks. The name café au lait is French for "coffee with milk" and refers to their light-brown color. They are caused by a collection of pigment-producing melanocytes in the epidermis of the skin. These spots are typically permanent and may grow or increase in number over time.

Dysplasia is any of various types of abnormal growth or development of cells or organs, and the abnormal histology or anatomical structure(s) resulting from such growth. Dysplasias on a mainly microscopic scale include epithelial dysplasia and fibrous dysplasia of bone. Dysplasias on a mainly macroscopic scale include hip dysplasia, myelodysplastic syndrome, and multicystic dysplastic kidney.

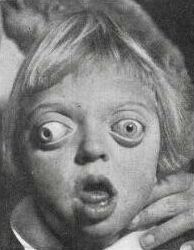
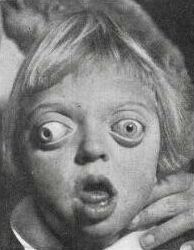
Cherubism is a rare genetic disorder that causes prominence in the lower portion in the face. The name is derived from the temporary chubby-cheeked resemblance to putti, the chubby-faced infants featured in Renaissance paintings, which were often mistakenly described as cherubs.
Polyostotic fibrous dysplasia is a form of fibrous dysplasia affecting more than one bone. Fibrous dysplasia is a disorder where bone is replaced by fibrous tissue, leading to weak bones, uneven growth, and deformity.

McCune–Albright syndrome is a complex genetic disorder affecting the bone, skin and endocrine systems. It is a mosaic disease arising from somatic activating mutations in GNAS, which encodes the alpha-subunit of the Gs heterotrimeric G protein.
Cleidocranial dysostosis (CCD), also called cleidocranial dysplasia, is a birth defect that mostly affects the bones and teeth. The collarbones are typically either poorly developed or absent, which allows the shoulders to be brought close together. The front of the skull often does not close until later, and those affected are often shorter than average. Other symptoms may include a prominent forehead, wide set eyes, abnormal teeth, and a flat nose. Symptoms vary among people; however, intelligence is typically unaffected.

GNAS complex locus is a gene locus in humans. Its main product is the heterotrimeric G-protein alpha subunit Gs-α, a key component of G protein-coupled receptor-regulated adenylyl cyclase signal transduction pathways. GNAS stands for Guanine Nucleotide binding protein, Alpha Stimulating activity polypeptide.
Osteochondrodysplasia is a general term for a disorder of the development (dysplasia) of bone ("osteo") and cartilage ("chondro"). Osteochondrodysplasias are rare diseases. About 1 in 5,000 babies are born with some type of skeletal dysplasia. Nonetheless, if taken collectively, genetic skeletal dysplasias or osteochondrodysplasias comprise a recognizable group of genetically determined disorders with generalized skeletal affection. Osteochondrodysplasias can result in marked functional limitation and even mortality.

Ollier disease is a rare sporadic nonhereditary skeletal disorder in which typically benign cartilaginous tumors (enchondromas) develop near the growth plate cartilage. This is caused by cartilage rests that grow and reside within the metaphysis or diaphysis and eventually mineralize over time to form multiple enchondromas. Key signs of the disorder include asymmetry and shortening of the limb as well as an increased thickness of the bone margin. These symptoms are typically first visible during early childhood with the mean age of diagnosis being 13 years of age. Many patients with Ollier disease are prone to develop other malignancies including bone sarcomas that necessitate treatment and the removal of malignant bone neoplasm. Cases in patients with Ollier disease has shown a link to IDH1, IDH2, and PTH1R gene mutations. Currently, there are no forms of treatment for the underlying condition of Ollier disease but complications such as fractures, deformities, malignancies that arise from it can be treated through surgical procedures. The prevalence of this condition is estimated at around 1 in 100,000. It is unclear whether the men or women are more affected by this disorder due to conflicting case studies.

Pseudoachondroplasia is an inherited disorder of bone growth. It is a genetic autosomal dominant disorder. It is generally not discovered until 2–3 years of age, since growth is normal at first. Pseudoachondroplasia is usually first detected by a drop of linear growth in contrast to peers, a waddling gait or arising lower limb deformities.
Bone disease refers to the medical conditions which affect the bone.
Monostotic fibrous dysplasia is a form of fibrous dysplasia where only one bone is involved. It comprises a majority of the cases of fibrous dysplasia.
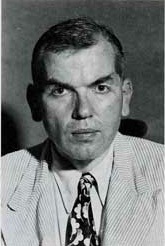
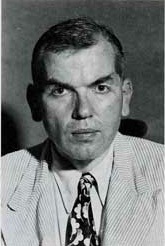
Fuller Albright was an American endocrinologist who made numerous contributions to his field, especially to the area of calcium metabolism. Albright made great strides and contributions to the understanding of disorders associated with calcium and phosphate abnormalities in the body. He also was a published author and in his books he detailed his findings.
In medical contexts, a facies is a distinctive facial expression or appearance associated with a specific medical condition. The term comes from Latin for "face". As a fifth declension noun, facies can be both singular and plural.

Orthopedic surgery is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal injuries, sports injuries, degenerative diseases, infections, bone tumours, and congenital limb deformities. Trauma surgery and traumatology is a sub-specialty dealing with the operative management of fractures, major trauma and the multiply-injured patient.
Craniofacial regeneration refers to the biological process by which the skull and face regrow to heal an injury. This page covers birth defects and injuries related to the craniofacial region, the mechanisms behind the regeneration, the medical application of these processes, and the scientific research conducted on this specific regeneration. This regeneration is not to be confused with tooth regeneration. Craniofacial regrowth is broadly related to the mechanisms of general bone healing.

Calvarial doughnut lesions-bone fragility syndrome, also known as familial calvarial doughnut lesions, is a rare autosomal dominant genetic disorder characterized by mild to moderate fragility of the bones accompanied with calvarial doughnut lesions.